Government
Sweet 16 and counting for stem cell clinical trial
Dr. Judy Shizuru: Photo courtesy Jasper Therapeutics Over the years the California Institute for Regenerative Medicine (CIRM) has invested a lot in helping…

Dr. Judy Shizuru: Photo courtesy Jasper Therapeutics
Over the years the California Institute for Regenerative Medicine (CIRM) has invested a lot in helping children born with severe combined immunodeficiency (SCID), a fatal immune disorder. And we have seen great results with some researchers reporting a 95 percent success rate in curing these children.
Now there’s more encouraging news from a CIRM-funded clinical trial with Jasper Therapeutics. They have announced that they have tested their approach in 16 patients, with encouraging results and no serious adverse events.
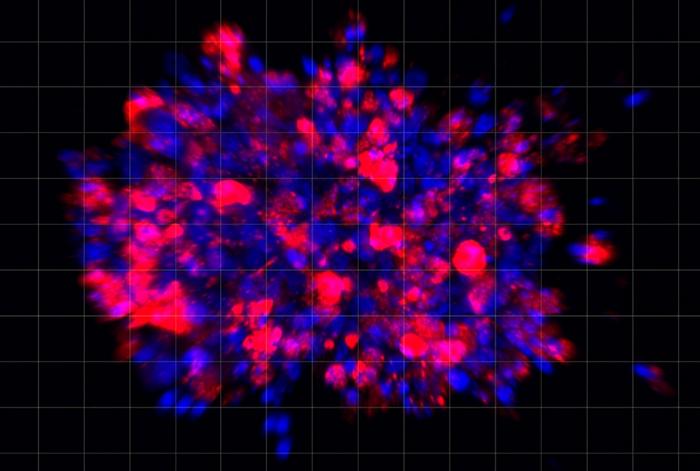
Let’s back up a little. Children born with SCID have no functioning immune system, so even a simple infection can prove life threatening. Left untreated, children with SCID often die in the first few years of life. Several of the approaches CIRM has funded use the child’s own blood stem cells to help fix the problem. But at Jasper Therapeutics they are using another approach. They use a bone marrow or hematopoietic stem cell transplant (HCT). This replaces the child’s own blood supply with one that is free of the SCID mutation, which helps restore their immune system.
However, there’s a problem. Most bone marrow transplants use chemotherapy or radiation to destroy the patient’s own unhealthy blood stem cells and make room for the new, healthy ones. It can be effective, but it is also toxic and complex and can only be performed by specialized teams in major medical centers, making access particularly difficult for poor and underserved communities.
To get around that problem Jasper Therapeutics is using an antibody called JSP191 – developed with CIRM funding – that directs the patient’s own immune cells to kill diseased blood stem cells, creating room to transplant new, healthy cells. To date the therapy has already been tested in 16 SCID patients.
In addition to treating 16 patients treated without any apparent problems, Jasper has also been granted Fast Track Designation by the US Food and Drug Administration. This can help speed up the review of treatments that target serious unmet conditions. They’ve also been granted both Orphan and Rare Pediatric Disease designations. Orphan drug designation qualifies sponsors for incentives such as tax credits for clinical trials. Rare Pediatric Disease designation means that if the FDA does eventually approve JSP191, then Jasper can apply to receive a priority review of an application to use the product for a different disease, such as someone who is getting a bone marrow transplant for sickle cell disease or severe auto immune diseases.
In a news release, Ronald Martell, President and CEO of Jasper Therapeutics said:
“The FDA’s Fast Track designation granted for JSP191 in Severe Combined Immunodeficiency (SCID) reinforces the large unmet medical need for patients with this serious disease. Along with its previous designations of Orphan and Rare Pediatric Disease for JSP191, the FDA’s Fast Track recognizes JSP191’s potential role in improving clinical outcomes for SCID patients, many of whom are too fragile to tolerate the toxic chemotherapy doses typically used in a transplant.”
therapeutics
stem cells
medical
application
therapy
fda
clinical trials

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…