Digital Health
Study: Increased Transparency Between Payers and Providers at the Point-of-Care Improves Risk Capture and Quality Measures
What You Should Know: – IllumiCare, a pioneer in point-of-care healthcare information technology, today released a new report detailing how increased…

What You Should Know:
– IllumiCare, a pioneer in point-of-care healthcare information technology, today released a new report detailing how increased data transparency between health plans and providers on care and coding gaps results in higher compliance, process improvement, and positive behavior changes among network providers.
– The report demonstrates, across multiple plans, that placing previously unavailable yet actionable information on quality gaps, HCC (Hierarchical Condition Categories) capture, HRA completion and other initiatives, within the provider’s workflow, is effective in closing more gaps.
Improving Quality of Care Via Increasing Data Transparency
Over the seven-month period, a large Medicare Advantage plan used the Ribbon to focus on quality measures and saw a 342% net increase in users achieving a 4+ star rating, outpacing their peers. The Ribbon users went from seven to 31% achieving 4+ stars, while the non-users went from 10% to 20%. From a risk capture perspective, another plan used the platform to observe and increase HCC capture, finding the process of coding more manageable and enforceable, resulting in an increase of 25% in recapture rates.
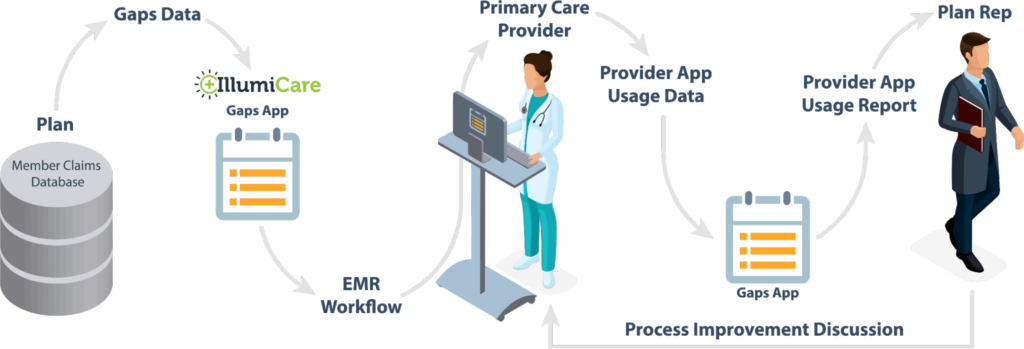
IllumiCare’s Smart Ribbon is an EMR-agnostic platform of clinical apps that requires no separate login, patient lookup or EMR integration. The platform places care and coding requirements and information from the plan conveniently in front of primary care physicians (PCPs) during their normal workflow. It “nudges” them in their workflow as to any care and coding gaps that may exist for the patient, so they can “close the loop.”
The report demonstrates the advantage of making a plan’s gaps data more transparent to the provider at the point-of-care, while also making the provider’s interactions with that data transparent to the plan. This two-sided transparency creates an enforcement loop that eliminates the majority of a practice’s reasoning for not moving the needle in process efficiency.
“Too many solutions are only focused on delivering the data, but that’s just the start. The most compelling insight from this data is the clear opportunity for behavior change and how plans can work alongside providers to enable it long-term,” said G.T. LaBorde, CEO of IllumiCare. “This opportunity to enact change through a complete feedback loop has not existed before. The provider has clarity on all care needs and the health plan knows who uses the program, when they use it and what they do with it. This is invaluable to improving care for members across networks.”

Keep it Short
By KIM BELLARD OK, I admit it: I’m on Facebook. I still use Twitter – whoops, I mean X. I have an Instagram account but don’t think I’ve ever posted….
Asian Fund for Cancer Research announces Degron Therapeutics as the 2023 BRACE Award Venture Competition Winner
The Asian Fund for Cancer Research (AFCR) is pleased to announce that Degron Therapeutics was selected as the winner of the 2023 BRACE Award Venture Competition….
Seattle startup Olamedi building platform to automate health clinic communications
A new Seattle startup led by co-founders with experience in health tech is aiming to automate communication processes for healthcare clinics with its software…













