Government
Data: Key to Unlocking Better Behavioral Health Outcomes
The growing demand for behavioral healthcare in America is putting a serious strain on both payers and providers with no signs of slowing down anytime…


The growing demand for behavioral healthcare in America is putting a serious strain on both payers and providers with no signs of slowing down anytime soon. A report from Mental Health America found that one in five U.S. adults has a mental illness. Furthermore, concerns around the state of youth mental health, which exploded during the pandemic, continue to grow at an alarming rate. A recent Pew Research study found children’s mental health is the most concerning issue among parents in 2023. Earlier this month, the U.S. Surgeon General released a report raising the alarm about an epidemic of loneliness in the U.S.
While the need for expanded access to care has become increasingly obvious, our ability to meet that need is, unfortunately, not trending in the right direction. The U.S. Department of Health and Human Services has estimated that by 2025 the nation will have 10,000 fewer mental health professionals than it needs. At the same time, Mental Health America’s survey finds that almost 30% of U.S. adults with mental health issues do not receive treatment.
With increasing demand for care and a decreasing supply of providers, every part of the behavioral health ecosystem needs to work more efficiently – and using data more effectively is one way to make it happen. Payers that implement innovative uses of data and technology can offer their members easier access to higher-quality care that better fits their needs, while simultaneously improving operations and business performance. Here are a few places where data can help improve behavioral healthcare for everyone.
Building member cohorts and segment-specific approaches
Payers can expedite and improve the process of evaluating members seeking care by analyzing historical claims across a population and using it alongside other third-party research. This data and information can enable payers to understand commonalities between the challenges different people face and the best paths to positive outcomes. By applying the knowledge payers gain from historical claims and research to the data they have about current members seeking care, payers can very quickly develop a good idea of where a member falls on the acuity spectrum and the type of care that will best suit their needs. They can also use this data to proactively connect members with services they may benefit from, ultimately improving outcomes while driving compliance. Vendors and data scientists can work with payers to create algorithms that further optimize care.
Data can play an important role in improving behavioral health access and outcomes from the moment a member engages with their health plan to seek care. Streamlining this process ultimately helps minimize stress for people seeking care and accelerates their path to positive outcomes.
Improving Provider Network Management
Payers can improve member experiences by exploring and adopting better processes and technology for managing their database of in-network providers. Ensuring the database is consistently updated with correct contact information, areas of expertise, and status on accepting new patients, will decrease the number of obstacles members encounter when seeking care. Additionally, if data on topics like a provider’s specialty and expertise is included and kept current, payers can use it alongside insight gained by analyzing claims during the member screening process. In addition to using technology to streamline access to care, it can also be leveraged to match members with the right providers. Ensuring that members are matched to providers who understand their experiences when it comes to culture, ethnicity, race, and/or LGBTQIA+ identity is an important factor in successful treatment outcomes. Embracing data gives payers the insights they need to ensure their network adequately covers the scope of culturally competent specialized care their member population needs while managing trends in demand over time.
Streamlining Scheduling
Embracing data and technology can help payers and providers work together to overcome scheduling challenges. If providers give payers real-time visibility into their scheduling systems, and capabilities to book appointments during available times, members can be scheduled for an appointment immediately – even during the first interaction with their health plan. Speeding up the pathway to care significantly increases the chances that a member will follow through with getting the care they need, further improving outcomes.
Measuring Care & Outcomes
Beyond improving behavioral health by addressing issues around better, quicker access, data can also allow providers and patients to monitor progress. Setting and working towards concrete and measurable goals, and the positive influence of seeing progress as it happens will only accelerate a patient’s journey. From a payer’s perspective, measuring care and outcomes, and harnessing that data to better inform care pathways for members in the future will improve behavioral health offerings over time. For example, knowing which providers are effective across diagnoses can better inform the referral process for new members seeking care. This knowledge can also help payers ensure the providers across their networks are adequately meeting member needs.
Demand for behavioral healthcare has greatly outpaced supply, stressing health plans and provider networks, and failing many patients. By rethinking their approaches and using data and technology in new ways, health plans can quickly connect members with care – and ensure they’re getting the right care – to strengthen quality and outcomes.
About Sarah Reilly, SVP, Product and Strategy, Lucet
Sarah Reilly joined Lucet in September 2021 as senior vice president of strategy, product, and innovation. With over 20 years of professional experience, Sarah is skilled in commercialization, healthcare strategy, and business transformation. Before joining Lucet, she was vice president of strategic partnerships at Magellan Health, where she oversaw strategic enterprise partnerships and led business strategy. Prior to this position, she led market access initiatives across several digital platforms at Verily.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
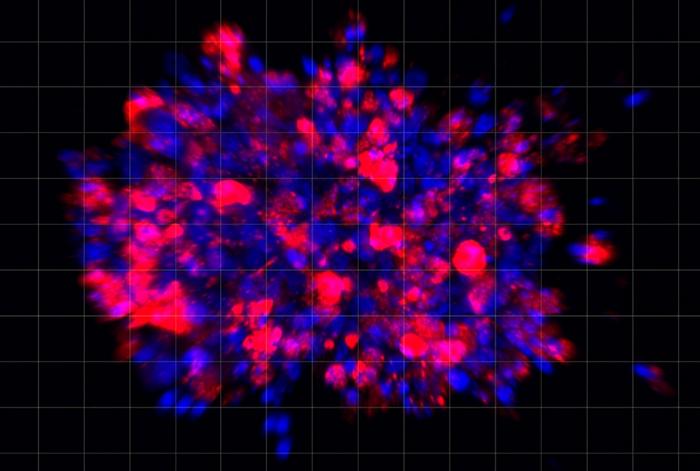
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…