Government
Doctors inclined to prescribe new Alzheimer’s drug despite concerns
Doctors who treat Alzheimer’s patients say they’re likely to prescribe Eisai and Biogen’s new therapy approved Friday, but sounded notes of caution…

Doctors who treat Alzheimer’s patients say they’re likely to prescribe Eisai and Biogen’s new therapy approved Friday, but sounded notes of caution over the lack of insurance coverage for the drug and a number of worrying side effects, including several reports of patient deaths.
The drug, which was known as lecanemab and will be sold under the brand name Leqembi, reduced the rate of cognitive decline by 27% in a study of nearly 1,800 people with early-stage Alzheimer’s, offering new hope after decades of failed clinical trials and controversy surrounding the approval of Aduhelm in 2021. The results, doctors stated, make the drug an option for patients like those in the trial, with mild cognitive impairment and elevated levels of amyloid, a protein in the brain associated with Alzheimer’s.
 Erik Musiek
Erik Musiek“I see a lot of these people in my clinic, and it is very difficult to watch them decline,” said Erik Musiek, associate professor of neurology at Washington University School of Medicine in St. Louis. “Currently, we have very little to offer these people. I am optimistic that lecanemab could have a significant impact in this population.”
But other doctors believe the drug will have only moderate benefits or no meaningful effects. And reports of side effects further complicate the calculus over whether to prescribe, as highlighted by a Jan. 4 research letter in the New England Journal of Medicine that linked the death of a clinical trial participant to Leqembi.
It’s unclear whether the 65-year-old patient received Leqembi during the randomized portion of the clinical trial, but she took the drug during the open-label phase that provided the drug to all participants.
The patient later suffered a stroke, and was given an anti-clotting treatment, called tissue plasminogen activator, or t-PA. The combination of t-PA and lecanemab may have set off a fatal cascade of brain bleeding and hemorrhages, researchers at Northwestern University Feinberg School of Medicine said.
“The extensive number and variation in sizes of the cerebral hemorrhages in this patient would be unusual as a complication of t-PA solely related to cerebrovascular amyloid,” the research letter stated.
Northwestern neuropathologist Rudolph Castellani, one of the researchers who contributed to the letter, more explicitly pointed to Leqembi’s role in the death as part of a November article in Science.
“There’s zero doubt in my mind that this is a treatment-caused illness and death,” Castellani told Science. He declined an Endpoints News interview request.
 Marwan Sabbagh
Marwan SabbaghMarwan Sabbagh and Christopher van Dyck, who conducted the clinical trial, don’t believe there’s enough evidence to blame Leqembi for the death. They argued in an accompanying response letter in NEJM that t-PA treatments alone can cause fatal hemorrhages.
“There have been earlier reports of fatal large catastrophic intracerebral hemorrhages after t-PA treatment in persons with cerebral amyloid angiopathy (CAA) in the absence of any anti-amyloid medications,” stated the response.
Because of the death, doctors said they would be circumspect about prescribing Leqembi to patients on certain blood thinners and those like the woman with APOE4 genes that heighten the risk for side effects.
In the clinical trial, about one in five people who received Leqembi experienced an adverse event such as brain bleeding. Roughly 0.7% of participants in the Leqembi group and 0.8% of those in the placebo group died, reflecting six deaths in the Leqembi group and seven in the placebo group.
Eisai said in a news release that it would provide physicians with a summary of essential prescribing information and how to monitor patients for side effects like amyloid-related imaging abnormalities, which can be life-threatening.
But not all clinics have the infrastructure to assess whether patients are a good fit for Leqembi or can complete safety checks for patients after infusions.
“Doing this right, quite literally takes a village,” said Lon Schneider, an Alzheimer’s expert at the USC’s Keck School of Medicine.
Medicare coverage
As another complicating factor in prescription decisions, it doesn’t appear Medicare will cover the drug, at least anytime soon, and it’s unclear whether insurers will pay for it. Before prescribing, Schneider said his institution will gauge families’ ability to pay for not only the $26,000 treatment but the medical visits, the infusions, MRIs and other procedures necessary.
 Lon Schneider
Lon Schneider“There are plenty of people with early Alzheimer’s disease with families who can afford it, but the question would be, do they believe the cost is worthwhile,” Schneider said. “For others who cannot afford it, there is no equity.”
Musiek said he would prescribe the drug, but only once Medicare and insurers cover it. The FDA granted accelerated approval to the drug, and full approval may be required for these things to happen.
Some doctors expressed frustration that the drug isn’t part of Risk Evaluation and Mitigation Strategy, or REMS, an FDA program that beefs up safety monitoring requirements.
“When the topic is new drugs for Alzheimer’s disease, FDA is consistently irresponsible,” said Penn Memory Center co-director Jason Karlawish over the lack of a REMS program, but he added that he would still prescribe the drug under limited circumstances.
Some doctors say they’re more likely to prescribe Leqembi over Aduhelm because there is more evidence that the newly approved medicine works. Jeff Gelblum, neurologist at First Choice Neurology who is currently treating about 50 patients with Aduhelm, said he won’t switch patients off Aduhelm but will offer Leqembi to new patients.
“I’m grateful that we would now have two drugs in the same therapeutic space and it validates my treatment approach all along. I’ve always been a believer in amyloid reduction as a reasonable strategy to mitigate Alzheimer’s disease,” he said.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
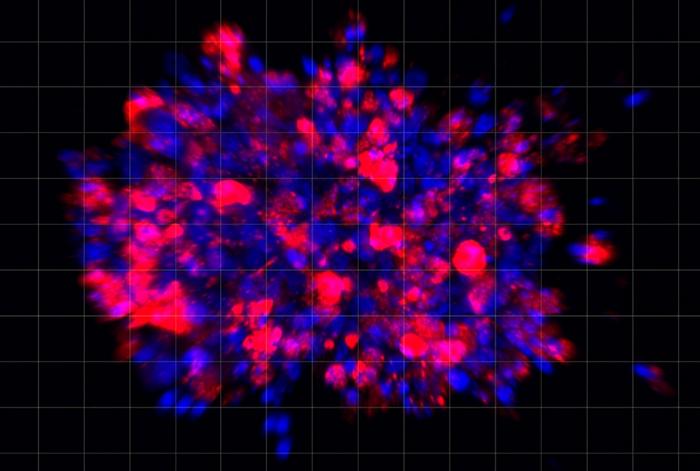
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…