Government
Enacting Care Coordination Policy to Curb the Drug Epidemic
Vatsala Kapur, Senior Director of Government Affairs at Bamboo Health The U.S. has reached a grim milestone with an estimated 107,622 drug overdose deaths…


The U.S. has reached a grim milestone with an estimated 107,622 drug overdose deaths in the United States during 2021. With a post-pandemic spotlight on mental health and substance use disorder challenges, Congress and the Biden administration are working on multiple plans to address these issues.
Earlier this year, the Biden Administration sent its first national drug control strategy to Congress, which focused on two pillars, one of which centered on addressing untreated addiction. This strategy is just the tip of the iceberg. As part of President Biden’s Mental Health Strategy, which was announced during his first State of the Union, the Department of Health and Human Services (HHS) awarded nearly $105 million to 54 states and territories as they prepared for the transition from the National Suicide Prevention Line to the 988 line this past July. A bipartisan group in Congress proposed the 988 Implementation Act, with the goal to increase access to behavioral health services, especially those in crisis through the three-digit number, akin to 911. Further, President Biden referenced the opioid epidemic and how imperative it is we beat it as a nation.
While we’re certainly headed in the right direction, enacting policy that promotes care coordination and supports behavioral health crisis management will be the next step in combatting substance use disorder in the United States. To meaningfully improve mental health care and outcomes, the federal government must take steps to integrate mental health information into our clinician’s workflows.
Currently, our country’s healthcare system operates in silos, separating physical care from mental care, even though they are interconnected. Now that the 988 line has launched, lack of care coordination is evident and will only further our country’s siloed system. Care coordination and integration is at the core of solving this issue, but we need our governments at the state and federal level to help facilitate this necessary change.
First, it’s important that the federal government make financial investments that aid in this integration. While physical health providers were eligible for federal financial incentives from the Health Information Technology for Economic and Clinical Health Act enacted as part of the American Recovery and Reinvestment Act of 2009 (P.L. 111-5), mental health providers were left out of the equation. To create meaningful change, the federal government must back this integration through financial means for both mental and physical health providers.
In addition to providing financial investment, our government must also consider how to balance policies that encourage care coordination and the unique privacy concerns related to mental health data. Currently, patient data – regardless of its relation to physical or mental health – can simply get stuck in our doctor’s offices. Providers often cannot share a patient’s medical history or even a list of current medications with other providers in a patient’s care team due to patient privacy concerns. This can become a significant issue when a patient has multiple providers for their behavioral and physical health conditions.
While patient privacy is of the utmost importance, it also can hinder care coordination, further separating the healthcare system into silos. In many instances, state privacy laws are more stringent than federal laws, meaning care coordination becomes even more limited depending on the state where care is delivered. Through policy, our state and federal governments must consider how to protect this data while allowing the exchange of information that could save lives, especially in crisis situations. This could be accomplished by urging state governments and partnering with them to adopt more unified guidelines for effective physician communications across the U.S.
While the recent focus by Congress and the Biden administration to address the nation’s substance use and mental health crisis is encouraging, there’s more work to be done. We must first enable an infrastructure for crisis management that supports our country’s growing behavioral health needs. By first offering financial investments and incentives and enacting policy that pushes care coordination and integration forward, our clinicians can focus on what matters most – caring for their patients.
About Vatsala Kapur
Vatsala Kapur, senior director of government affairs at Bamboo Health, has over two decades of experience in health policy and public health. Bamboo Health, formerly Appriss Health and PatientPing, is a healthcare technology solutions company focused on fostering care collaboration and providing information and actionable insights across the entire continuum of care.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
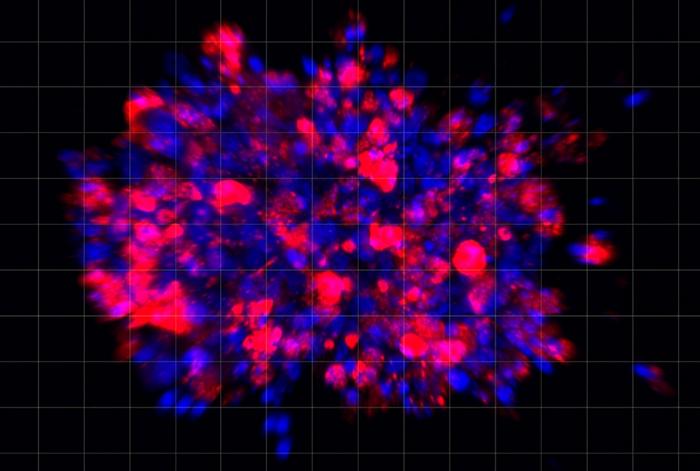
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…