Government
Fungus Shrinks to Get into the Brain
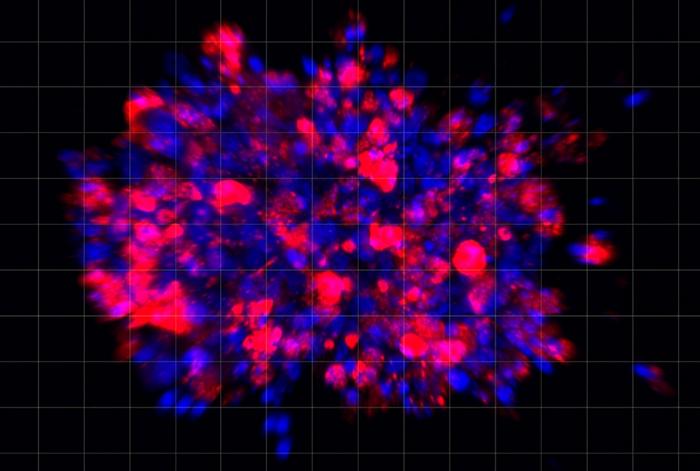
Scientists infected mice with various sizes of C. neoformans. They found that in comparison to medium and large cells, the smallest cells preferentially…
Researchers at the University of Utah (U of U) Health report that a fungus that is a common cause of fungal meningitis undergoes a transformation once it enters the body, allowing it to infect the brain. Studies in mice showed that as the fungal intruder travels through the body, it shrinks and acquires characteristics that help the infection to spread, all in a matter of days.
The discovery could lead to new strategies for blocking Cryptococcus neoformans infection and preventing detrimental effects on the host. C. neoformans is the leading cause of a rare but deadly swelling of the brain that occurs in people with weakened immune systems.
The university team published its study (“A dissemination-prone morphotype enhances extrapulmonary organ entry by the fungus Cryptococcus neoformans”) in Cell Host and Microbe.
“Environmental pathogens move from ecological niches to mammalian hosts, requiring adaptation to dramatically different environments. Microbes that disseminate farther, including the fungal meningitis pathogen C. neoformans, require additional adaptation to diverse tissues,” the investigators wrote.
“We demonstrate that the formation of a small C. neoformans morphotype—called ‘seed’ cells due to their colonizing ability—is critical for extrapulmonary organ entry. Seed cells exhibit changes in fungal cell size and surface expression that result in an enhanced macrophage update. Seed cell formation is triggered by environmental factors, including C. neoformans’ environmental niche, and pigeon guano with phosphate plays a central role.

“Seed cells show the enhanced expression of phosphate acquisition genes, and mutants unable to acquire phosphate fail to adopt the seed cell morphotype. Additionally, phosphate can be released by tissue damage, potentially establishing a feed-forward loop of seed cell formation and dissemination. Thus, C. neoformans’ size variation represent inducible morphotypes that change host interactions to facilitate microbe spread.”
“Cryptococcus cells in the lungs are diverse with different sizes and different appearances. So, when my graduate student showed me pictures of the uniformity of cells from the brain, I was shocked,” said Jessica Brown, PhD, associate professor of pathology at U of U Health and the study’s senior author. “It suggested that there was some very strong reason why only this population of cells were making it that far into the body.”
Fungus thrives in many different habitats
Brown’s fascination with the fungus came from the observation that it thrives in so many different habitats. In the wild, the organism lives in rotting wood and bird droppings. If it is inadvertently inhaled, the fungus can survive in the lungs and then travel in the bloodstream to the brain and other organs, each of which has its own challenging micro-environment.
Previously, other scientists found that the fungus copes with living in the lungs by growing to 10 times its normal size, presumably becoming too large for the host immune system to destroy. But in other parts of the body, fungal cells are much smaller. Brown wondered, could the cells’ extra-small size be another type of advantage? Perhaps that characteristic helps them colonize other organs, such as the brain.
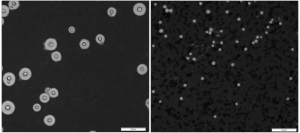
To find out, her team infected mice with various sizes of C. neoformans. They found that in comparison to medium and large cells, the smallest cells preferentially infected the brain. These cells were not only diminutive but differed in other ways. Compared to larger fungal cells, they had unique features on their surface that were similarly important for accessing the brain. They also turned on a different set of genes.
This evidence suggested that the small fungal cells, that Brown dubbed “seed” cells, were not just miniature versions of larger cells. They had undergone a wholesale change.
After searching for triggers, Brown’s group found that a specific chemical—phosphate—could induce the shift. Knowing that phosphate is released when tissue is damaged during infection, Brown speculates that the chemical accumulates in the lungs, the first site where fungi settle after entering the body. This allows the fungal cells to reconfigure themselves as seed cells, which enables the infection to spread further.
From bird guano to the brain
The fungi’s ability to effectively target the brain may have originated from a unique source: bird guano. C. neoformans thrive in pigeon droppings, which have high levels of the seed cell-triggering molecule, phosphate.
Brown thinks this could demonstrate how the fungus’ pathogenicity arose in the first place.
“We think that selective pressures from environmental niches like pigeon guano are somehow able to confer to C. neoformans the ability to infect mammals,” she said.
Regardless of how the fungus’ infectious property arose, Brown’s team is now trying to block that ability with FDA-approved drugs. They are determining whether there may be an existing compound that blocks C. neoformans from becoming seed cells that could provide a ready-to-go remedy for preventing or treating fungal meningitis.
The post Fungus Shrinks to Get into the Brain appeared first on GEN – Genetic Engineering and Biotechnology News.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…