Government
Investing in CAR T-cell therapy to treat cancer
The California Institute for Regenerative Medicine (CIRM) is investing $4 million to support Dr. William Murphy and UC Davis researchers to develop and…


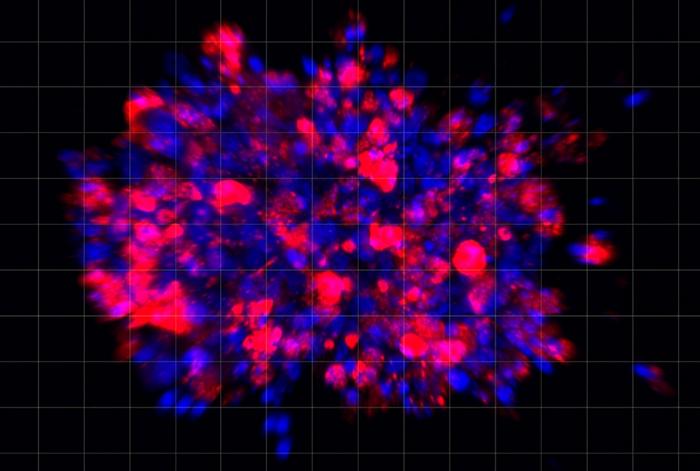
The California Institute for Regenerative Medicine (CIRM) is investing $4 million to support Dr. William Murphy and UC Davis researchers to develop and test a chimeric antigen receptor (CAR) T-cell therapy to treat various B-cell malignancies, ranging from lymphomas to leukemias.
In this Q&A—courtesy of UC Davis Health—Dr. Murphy discusses the importance of T-cell therapy and its implications for developing cancer treatments. His work is a collaboration between CIRM, the nonprofit organization Caring Cross, and UC Davis Health.
What are B-cell malignancies?
B-cells are a type of white blood cells that make antibodies. They are key to the body’s immune system. When healthy B-cells change into fast-growing cancer cells that don’t die, they cause B-cell malignancies.
This can affect people at different ages. They may show up in children as B-cell acute lymphoblastic leukemia (B-ALL), an aggressive blood and bone marrow cancer. In adults, they make up about 85% of non-Hodgkin lymphoma (NHL), a cancer that starts in B lymphocytes. In the elderly, B-cell malignancies may come as multiple myeloma, a cancer of the plasma cells.
There are different lines of treatments for B-cell lymphoma and leukemia, including immunotherapy using chimeric antigen receptor (CAR) T cells. These cells have revolutionized cancer treatment since they have been shown to work, and cure, when nothing else can.
What is chimeric antigen receptor (CAR) T-cell therapy?
Chimeric antigen receptor (CAR) T-cell therapy uses the body’s own defenses to fight disease. It is a new and exciting form of immunotherapy that works by modifying the receptors of immune cells (T cells) involving antibodies to target specific cancers, such as leukemias and lymphomas.
CAR T cells are being used to treat some blood cancers with long-term success. The U.S. Food and Drug Administration (FDA) first approved CAR T-cell therapy in 2017. Their use is growing rapidly and being applied to other tumor types. Yet, this therapy is extremely expensive, even with insurance. It’s also a very intensive procedure and it takes time to generate the CAR T cells from the patient.
While it could be considered a game changer, one of the issues with this therapy is the case relapse rate. The big holy grail in cancer therapy is how to prevent tumors from evading or escaping the immune attack. Around 60% of patients who get CAR therapy see their cancer return. If we can get the relapse rate down to negligible, that would be a tremendous advance.
How do you intend to use CAR products to reduce cancer relapse?
In CAR therapy, we take the immune T cells from a patient and use gene therapy to give a new receptor to signal and direct the T cell. The receptor usually has an antibody that recognizes a particular tumor antigen. Current FDA-approved CAR T therapies only target one tumor antigen.
CARs have had tremendous success. However, there is significant patient relapse because the tumor adapts and may lose that one antigen that we are targeting, allowing it to escape the treatment. Our strategy is to target multiple antigens to reduce the potential for relapse since the tumor cannot adapt that quickly.
We are also proposing a novel vector that will carry a CAR product, known as DuoCAR, that targets three antigens at the same time. As long as the tumor has one of the three antigens, then there’s little chance for the tumor to escape all three antibodies. This is similar to when you think about HIV treatment with the triple-drug therapy, where one alone is not sufficient.
The hope is that the 60 to 70% of the population who would have relapsed if they had the original CAR T cell treatment, would have a home run with our kind of treatment or product.
So, is this treatment for cancer patients who have relapsed?
We see this product as a new frontline therapy and not just for patients who relapse. What the patient has to go through in order for CAR T therapy to work is very strenuous. So, yes, if there are relapsed patients, they can be given DuoCAR, but we’re also hoping this will become the new standard of care, replacing the other CARs in the future for everyone.
To read the full Q&A, click here.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…