Government
Q/A: Podimetrics CEO Talks Preventing Diabetic Amputations
Diabetes prevention is one of the biggest challenges in the healthcare industry as more than 37 million Americans (11.3% of the population) suffer from…


Diabetes prevention is one of the biggest challenges in the healthcare industry as more than 37 million Americans (11.3% of the population) suffer from this debilitating chronic disease. As we close the year out, we sat down with Jon Bloom, MD, CEO and Co-founder of diabetic healthcare tech company Podimetrics to learn how the industry and his company are working to implement health equity change to serve patients living with advanced diabetes. The company’s FDA-cleared SmartMat provides a simple, in-home touchpoint to help stop diabetic foot complications.
Why are racial and ethnic minority populations continuing to experience adverse impacts from complex diabetes more so than other groups of patients?
Jon Bloom, M.D., CEO of Podimetrics: More than 154,000 diabetic amputations occur each year, and up to 80% of people who undergo an amputation will die within five years of the procedure. The risk of amputation is especially high for racial and ethnic minority populations living with type 2 diabetes. For example, Black people are up to 4x more likely to suffer from an amputation resulting from diabetic complications — and Indigenous people are up to 2x more likely.
A recent consumer survey also uncovered findings that reinforce the serious disparity problems facing minority populations that have been diagnosed with type 2 diabetes. For instance, Black respondents were more likely (31%) to have experienced a medical emergency because of complications from diabetes compared to the full survey sample (25%). The survey also found that Hispanic individuals with type 2 diabetes are increasingly being impacted by the challenges and disparities created by living with the condition, including 67% reporting mental health issues (compared to 50% for the broader sample) and 65% fearing type 2 diabetes would cause their death (compared to 53% for the broader sample).
High amputation rates tend to be clustered geographically in areas with high scores on the CDC Social Vulnerability Index and the heaviest concentrations of Black Americans. These areas, many of which are in the Deep South, map directly to known food deserts, pharmacy deserts, designated healthcare provider shortage areas, and lower rates of health literacy. Without access to healthy foods to prevent diabetes, pharmacies to access medications, or qualified primary and specialty care providers to prevent or treat the condition as it develops, residents of these areas don’t have the tools to manage diabetes. As a result, amputation may become the only option.
What changes can be made in the near term to address this health equity challenge?
Bloom: To succeed in reducing unnecessary amputations related to complex diabetes, our team knew we needed to launch a dedicated initiative that combines policy levers, reimbursement strategies, technical innovation, and boots-on-the-ground care to move forward with the ultimate goal of reducing the need for amputations among at-risk populations living with complex diabetes. That’s why we collaborated with the American Diabetes Association just this past year to launch the Amputation Prevention Alliance.
Success for the Alliance — which is focused specifically on addressing health equity challenges — comes down to reducing the more than 154,000 amputations that occur every year in the U.S. Some of the best ways to help prevent amputations and diabetic foot ulcers (DFUs) in people — including those who are racial and ethnic minorities — living with complex diabetes are as follows:
– Patient education (and clinician education) about the signs and symptoms associated with DFUs and diabetic neuropathy;
– Regular patient checkups, including appointments with a podiatrist, that are focused primarily on foot health; and
– Regulatory changes that include screening coverage for those most likely to be at risk of Peripheral Artery Disease (PAD).
Why is preventive care still so challenging today when it comes to diabetes?
Bloom: Preventive care for chronic diseases, such as diabetes, remains a challenge today as we continue to make small strides in the move from fee-for-service to value-driven care.
As we look to power preventive care for people dealing with complications from diabetes, we’d be well-served to borrow some ideas from a playbook embraced in oncology care and treatment. In oncology, providers from across the care team huddle up as a tumor board, examining the patient’s condition from every angle and developing a holistic treatment plan together.
People with diabetes could benefit from a similarly coordinated, multidisciplinary, and preventive approach. When a patient is at risk for amputation resulting from something like a diabetic foot ulcer, their primary care physician might convene an “amputation board” with medical specialists, social workers, the patient themselves, caregivers, and others to take a closer look at comprehensive strategies for avoiding a devastating outcome. Previous studies have demonstrated that this type of multidisciplinary care can reduce major amputations by up to 80%, allowing many more people to avoid a traumatic and life-altering event.
What role is / can tech play in the prevention for patients living with complex diabetes?
Bloom: Technology can play a huge role when it comes to preventing devastating complications for people living with diabetes. The emergence of virtual care amid the pandemic is a prime example of how technology can help drive connections and collaboration between care teams and people living with chronic diseases — connections that can help identify health issues before they become full-blown diseases.
Also, our team has seen positive impact for the patient populations that are using our own home-based technology — the SmartMat — to detect signs of diabetic foot complications up to five weeks before they present clinically, allowing for early intervention. This type of technology-driven prevention for people living with advanced diabetes has been shown through clinical research to help eliminate 71% of amputations, reduce all-cause hospitalizations by 52%, and lessen emergency department visits by 40%.
Can you tell us more about Amputation Prevention Alliance, and what efforts will this group be focused on in 2023?
Bloom: Today, every three minutes in the U.S., a limb is amputated due to diabetes — and most are actually avoidable. Our team at Podimetrics has been fully committed to putting an end to unnecessary “Civil War”–style amputations for people dealing with diabetes for more than a decade, and our work with the American Diabetes Association is an extension of this important mission.
Our collaboration specific to the Amputation Prevention Alliance — which is an effort between Podimetrics, the American Diabetes Association, Abbott, Advanced Oxygen Therapy Inc., Cardiovascular Systems, Inc., and the Critical Limb Ischemia (CLI) Global Society — rose out of our shared desire to finally put an end to unnecessary amputations for those living with advanced diabetes.
This month and in the first half of 2023, the Alliance will be rolling out a series of educational sessions targeted at clinicians and people living with diabetes. As patients are pushed to take more ownership in their health and well-being, it’s critical that they know what signs and symptoms they need to be on the lookout for if they are living with diabetes. It’s critical for these folks to be informed and active, not passive, in their own care. Education on their disease and guidance on best practices — such as access to evidence-supported medical tools and technologies — is the first step in our effort to empower people living with diabetes.
Our education efforts will also be targeted at clinicians and helping to educate them on early detection and preventive care best practices, instead of traditional sick care. Many clinicians have been trained in fee-for-service best practices, so there is a fundamental shift in how clinicians think and operate that needs to be addressed. Preventing amputations requires a team-based collaborative approach. We’ll be working closely with a variety of physician groups and alliances to broaden our education efforts through the Alliance in 2023.
Next year, the Amputation Prevention Alliance will also be tackling regulatory changes needed to ensure equity in care for all people living with diabetes — with a focus on driving new regulations that power preventive measures, such as facilitating additional research on amputation prevention, quality services performed by a podiatrist, and increased screening for issues such as peripheral artery disease.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
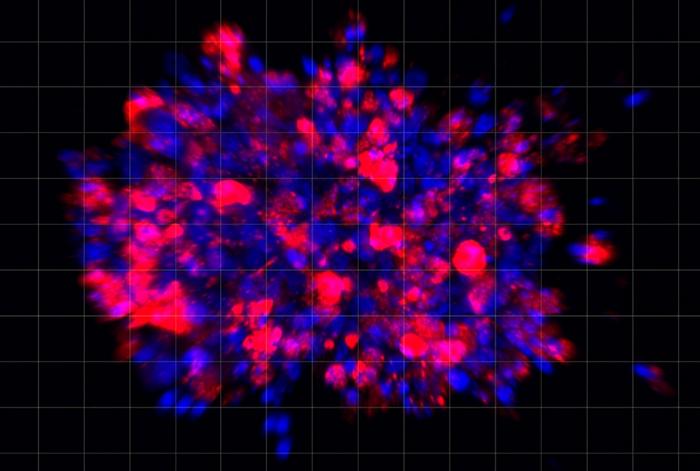
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…