Government
Social determinants of health: Making an impact
One of the advantages of leveraging behavioral science in healthcare marketing is that it provides marketers with powerful tools to do what we do best:…

Social determinants of health: Making an impact
By Mindy Vulpis, Ph.D.
One of the advantages of leveraging behavioral science in healthcare marketing is that it provides marketers with powerful tools to do what we do best: solve problems. Once we are able to identify the unique behavioral barriers at play, the science leads us toward solutions that are likely to be successful in addressing them. In this regard, behavioral strategizing is both elegant and satisfying.
But what happens when we are faced with behavioral challenges that are not so clearly solvable? This is often the case when we are approached by clients who are interested in addressing larger, societal-level problems through marketing. Specifically, pharma companies are focusing on their role in addressing social determinants of health (SDOH), and they are turning to their agency partners for help.
That brings us to the question: What can marketers do to address problems that seem so overwhelming and out of reach?
It’s true that these problems are complex. But that doesn’t mean there isn’t room – significant room – to make an impact.
Understanding the problem
Our clients are sometimes surprised when we tell them that SDOH aren’t really about diversity or inclusion, as important as those things are. Of course, it’s extremely important for people of all backgrounds to see themselves in marketing imagery so that they can feel valued and perceive that the associated messaging is speaking to them. But the pharma industry has recognized this need and has taken clear steps to address it in recent years.
To get a better understanding of what SDOH are about, let’s start with some definitions. SDOH are conditions in the places where people live, learn, and work that affect a wide range of health risks and outcomes.1 Usually, when people talk about SDOH, they are referring to health disparities or health inequities between different social groups.
A health inequity (or health disparity) is a type of difference in health in which disadvantaged social groups – such as racial/ethnic minorities, women, people living in poverty, or other groups who have persistently experienced social disadvantage or discrimination – systematically experience worse health outcomes or greater health risks than more advantaged social groups.2
Digging deeper to understand the “why”
When we think about solving for the challenges presented by SDOH, we can start in the same place as when we think about individual-level behavioral challenges: by digging deeper into the “Why?” In this case, why are historically disadvantaged groups continuing to experience significantly poorer outcomes? At their core, health inequities stem from two vexing and longstanding challenges: access and discrimination.
Access

While behavioral science traditionally focuses on understanding and changing individual health behaviors, a Social Determinants of Health approach widens that lens to look at the social and environmental factors that can also impact a person’s health.
Health disparities arise from different groups’ ability to access social and economic opportunities, as well as differences in the resources and support that they have available to them in their homes and neighborhoods.3 Reducing these inequalities requires large-scale structural changes to our institutions that are certainly beyond the grasp of any one agency or pharma company. But what we can do is identify and address the barriers to care that are created by these differences.
For example, years of research show that people living in poverty have reduced access to things such as jobs with health benefits and paid time off, high-quality health education and outreach, reliable transportation, and quality childcare. These barriers mean that people living in poverty have a lower likelihood of being able to do what we know leads to better health outcomes: seeking or receiving preventative health care or early-stage disease care, accessing high-quality health care providers and facilities, keeping appointments and adhering to prescribed treatments, accessing quality health insurance, eating a healthy diet, getting adequate exercise, becoming health literate, and ultimately playing a more active role in their health care.
By leveraging SDOH research to learn more about what factors may be systematically causing poorer outcomes for certain groups – especially those factors that we can potentially influence – we can try to intervene in ways that minimize the effects of these disadvantages.
Discrimination
Beyond access, it is also important to understand that not all racial, ethnic, or socioeconomic groups have similar experiences with the health care system. Historic and systematic discrimination has resulted in substantially differing levels of trust, communication, and self-advocacy among different groups, and these factors drive patients’ behavior in ways that impact health outcomes. Volumes of research literature have explored how various groups have been treated differently when seeking health care, but continued discrimination is not a foregone conclusion. We can assume that, at least today, discrimination is most often unintentional, the result of things like implicit bias or a lack of cultural competence (topics for another article), both of which come with being human but can be mitigated through awareness education.
Helping healthcare providers and health systems to identify and ultimately reduce their implicit biases (while increasing their cultural competence) could make a significant difference when it comes to ensuring that things like race, ethnicity, gender, or sexuality do not impact the type or quality of care that an individual receives.
What can we do?
Societal-level problems require societal-level solutions, but that doesn’t mean that we are helpless to support individuals who bear the brunt of health inequities. While pharma companies and marketers may not be able to fix the root cause of social problems, we can – and should – act to minimize their impact. Toward that end, the following are some ways to get started.
- Clarify what problem you are looking to solve. While addressing SDOH can feel overwhelming, a good first step is to start asking questions. Are you looking to increase diversity and inclusion, or are you wanting to meaningfully address barriers that are preventing disadvantaged populations from accessing care? Are you looking to address health inequity broadly, or is there a specific target population you are looking to engage? Are you looking to intervene early in the patient journey to help increase access to things like patient education and disease screening, or are you looking to help already-diagnosed patients get on treatment or become more adherent?
- Identify how and when social forces like access and discrimination may be affecting individual behavior. Behavioral science provides a great roadmap for addressing individual-
level behaviors, but we should also look beyond the individual level when trying to understand why people do what they do. We can understand human behavior in much greater depth when we view it with a human dynamics lens – understanding the patient as a whole person, in the context of their environment and relationships. That’s why it’s important to take a broad lens to the “Why?” every time we try to understand or impact patients’ motivation. This will enable us to learn not only what patients want to do, but also what they are able to do based on their circumstances. - Partner when possible. When it comes to reaching disadvantaged populations, it’s often not necessary – and not even advisable – to start from scratch. Grassroots organizations that are in underserved communities have deep knowledge about populations you are trying to reach, so they are in the best position to understand and share the most effective ways to make an impact. Leveraging these relationships may also help build trust with these vulnerable communities. Reach out to them and partner when you can.
- Understand cultural differences but be wary of stereotyping. It is critically important for both marketers and HCPs to become aware of the tendencies for different cultural groups to view or experience things differently than they might. This will enable them to tailor communications accordingly where appropriate. But this also makes it easy to fall into the tendency to stereotype, and that slope is slippery. There’s no easy solution for this, but awareness is a good first step when it comes to both patient outreach and HCP education.
Since problems around SDOH can be large and daunting, it’s helpful to start by thinking strategically about what can or cannot be impacted so that resources can be used efficiently toward meeting goals. Ultimately, addressing health inequities within a marketing environment will be a business decision, but thankfully, it is often the case that what’s best for patients is also best for business. Finding those synergies is the best way to ensure desirable outcomes for all.
References
- https://www.cdc.gov/socialdeterminants/index.htm
- Braverman. Ann Rev Pub Health. 2006;27:167-194.
- https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
Mindy Vulpis, Ph.D., is senior behavioral strategist at Evoke MicroMass.

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
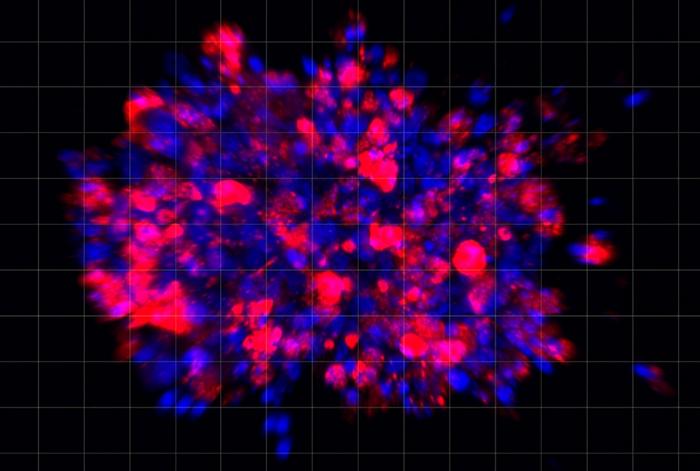
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…