With the help of a new grant from the National Institute of Health for more than $2.6 million, Assistant Professor Timothy Huang, Ph.D., will continue his research on the role of the brain’s immune cells on the risk of developing Alzheimer’s disease.
Alzheimer’s disease affects more than 47 million people worldwide, with 10 million new cases of dementia diagnosed each year. This number will continue to grow as the world population ages. Newly approved FDA treatments for Alzheimer’s remove beta-amyloid, a protein that accumulates into plaques, from the brain. However, these drugs are not a cure, and they don’t reverse the loss of memory and impaired cognition associated with Alzheimer’s disease.
“The key to finding effective ways to prevent and treat Alzheimer’s is digging deeper into the molecular aspects related to pathology and determining which changes may cause Alzheimer’s and which are a result of the disease,” says Huang. “This award will help us learn more about the link between genetic variants of TREM2—a key protein found in the brain’s immune cells—and the risk of developing Alzheimer’s.”
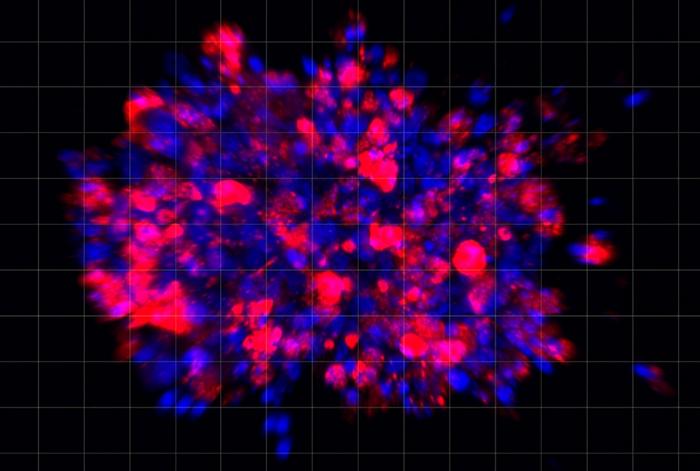
Huang’s research will focus on the puzzling observation that a rare genetic variant of TREM2 potentially reduces levels of beta-amyloid but is nonetheless associated with an increased risk of disease in some individuals. His team will investigate the possibility that the genetic variant produces its deleterious effects on tau—a toxic protein that accumulates inside the brain’s synapses and compromises the transmission of signals from one neuron to another.
“Results from this study will allow us to better understand how an Alzheimer’s disease risk factor can reduce beta-amyloid levels, which are thought to be protective, yet increase the risk of disease onset,” says Huang. “Since new treatments are focused on reducing amyloid levels, understanding how TREM2 genetic variants can reduce beta-amyloid yet confer increased risk of disease may give us further insight into improved or complementary drug treatments in the future.”
The grant, awarded by the National Institute on Aging of the National Institutes of Health, is “Molecular pathobiology of soluble TREM2 in Alzheimer’s disease,” Award number: RF1 AG056130-06.