Government
Alzheimer’s drug Leqembi gets full approval from FDA, allowing Medicare coverage
For the first time in 20 years, the FDA has bestowed full approval on a drug to treat Alzheimer’s disease, opening the door to coverage for millions…

For the first time in 20 years, the FDA has bestowed full approval on a drug to treat Alzheimer’s disease, opening the door to coverage for millions of Medicare recipients.
While Eisai and Biogen’s drug Leqembi had been available since January after the FDA cleared it through the accelerated approval pathway, the lack of reimbursement from Medicare had been a major barrier for its uptake.
 Ivan Cheung
Ivan Cheung“Today is a triumph for the Alzheimer’s disease community after so many years of hard work by scientists, clinicians, and clinical trial participants,” Eisai’s US chairman and CEO Ivan Cheung told Endpoints News in an interview. “This is a very humbling moment. I personally wish this would have come many years earlier.”
It’s a historic moment for a field that’s known little but failure in scientists’ efforts to halt the memory-robbing disease. Yet many unanswered questions remain, especially how to balance the uncertainty around the therapy’s long-term benefits with the very real and immediate risks of brain bleeding and swelling the drug can cause in some patients.
Those side effects, which in a few cases have proven fatal, are detected as amyloid-related imaging abnormalities, or ARIA, on brain scans. Leqembi’s full approval comes with a black box warning noting that ARIA events occurred more frequently in people carrying two copies of the APOE4 gene — known to significantly increase the risk of developing Alzheimer’s.
The antibody drug has been shown to reduce amyloid plaques in the brain and slow the course of the disease, albeit modestly. And since almost all Alzheimer’s patients are older, full approval and coverage by Medicare is a crucial step, and the government will only reimburse the drug for people who are included in registries to track their outcomes. Eisai has projected the $26,500 per year treatment could reach $7 billion in global sales by 2030.
A statement from the Centers for Medicare & Medicaid Services said that patients would still be liable for covering 20% of the drug’s cost — the standard Medicare coinsurance — after meeting their deductible, meaning that patients could be on the hook for at least $5,300 a year, not including cost-sharing for other services required to receive the treatment.
 Alvaro Pascual-Leone
Alvaro Pascual-Leone“It’s not going to be the cure-all, but it can be a very meaningful adjunct to the treatment of some people,” Alvaro Pascual-Leone, a professor of neurology at Harvard Medical School and medical director at Wolk Center for Memory Health in Boston, told Endpoints. “But it’s going to be a relatively small number of people. And we want to make sure that we provide it to the right ones, and not put the wrong ones in danger.”
The CMS previously said that physicians would need to use a patient registry to track the demographics and outcomes of patients getting the drug. Although some advocacy groups have criticized that requirement, many neurologists support it.
“CMS is looking for very little, and any physician can easily comply because they will know the answers anyway from evaluating their patients,” Lon Schneider, a professor at the University of Southern California and director of the California Alzheimer’s Disease Center, told Endpoints.
“The registry is a good thing,” he added. “It’s not a burden.”
Excitement and controversy
The highly anticipated decision comes after two tumultuous years for Alzheimer’s drugmakers — and for Biogen in particular. The storied Cambridge, MA biotech’s drug Aduhelm won an accelerated approval in June 2021 based on data showing it reduced amyloid plaques in the brain, but conflicting results on whether it slowed cognitive decline.
Aduhelm’s approval spurred several members of the FDA’s neurological drug advisory committee to quit in protest, leaving the group’s numbers depleted to this day. Later the CMS said it wouldn’t cover the drug, or any amyloid-targeting antibodies, until the FDA granted them full approvals based on evidence that they offered clinical benefits.
Leqembi won an accelerated approval in January for people with mild cognitive impairment or mild dementia and evidence of amyloid pathology from a brain scan or spinal tap. The full approval was based on data from a large study showing that an 18-month course of the drug slowed a common measure of cognitive decline by 27%, compared with placebo infusions.
Unlike Aduhelm, Eisai’s much cleaner trial left far less room for doubt. Yet there’s still considerable debate over just how meaningful the drug’s effect will be for patients and their families.
 Lon Schneider
Lon Schneider“This is a medication that shows a very small effect, and one of the challenges is that we don’t know which individuals will benefit,” Schneider said.
When Leqembi got an accelerated approval, Harvard’s Pascual-Leone thought that patients, doctors, and the healthcare system weren’t prepared for this drug.
“I still feel that way, because arguably we don’t have any more experience or knowledge than we had back then,” he said.
Many patients and their families seem to misunderstand what the drug does, Pascual-Leone said. “You’re not going to improve by 27%. It’s that you may worsen a little slower than what you might have expected,” he said. Nonetheless, Pascual-Leone has a list of patients who consider that slowing meaningful.
“In my mind, it’s a very individual thing. I think the role of clinicians is to educate the patients and their families and empower them to make a decision,” Pascual-Leone said. “It may not be that meaningful for some people. But the value of making it six more months to be at your granddaughter’s wedding may be extremely important to some individuals.”
Watching for side effects
And there are ongoing questions about the drug’s side effects, in particular brain swelling and bleeding, which doctors believe are linked to at least three deaths.
In Leqembi’s Phase III study, 12.6% of patients who got the drug had signs of brain swelling and 17.3% had signs of brain bleeding, compared to 1.7% and 9% of those who got a placebo, respectively.
The boxed warning recommends, but doesn’t require, that doctors test patients for the APOE4 gene that raises the risk of ARIA, though people with those genes can still get the drug. Patients taking blood thinners, which some experts believe amplified the effects of ARIA and could be related to the deaths, are also eligible for Leqembi. The new label says to exercise caution if administering an anticoagulant, but otherwise leaves physicians and patients to solve Leqembi’s complex risk-benefit calculation themselves.
 Madhav Thambisetty
Madhav Thambisetty“I don’t think there’s been enough attention on the safety aspects,” Madhav Thambisetty, a neurologist at the National Institute on Aging, a division of the National Institutes of Health, told Endpoints. “Critical and important questions regarding safety have not been published.”
Although ARIA typically occurs within the first few months or so of treatment, the longer-term impacts of those incidents on a person’s cognition and function are unknown, Thambisetty said. “That is a big limitation,” he said.
Amyloid-targeting antibodies are also known to reduce brain volume, but the consequences of that accelerated shrinkage are unclear. “That’s a pretty glaring gap,” he added.
A shift in patient care and expectations
The treatment requires hourlong infusions every two weeks, indefinitely, and fairly frequent assessments to monitor for ARIA or other side effects. Not all medical centers will be equipped to offer these services, and not all patients may be ready for the time that the treatment takes.
Finding patients with two APOE4 copies will also add to what’s asked of physicians and patients. Thambisetty, who treats Alzheimer’s patients, said he believes that people with two copies of the APOE4 gene shouldn’t get the drug.
“Up until now there hasn’t been a reason for routine APOE testing in clinical practice,” Thambisetty said. “It’s going to require large-scale genetic counseling,” not just for patients but also regarding children who may carry the gene.
Michael Irizarry, Eisai’s deputy chief clinical officer for Alzheimer’s disease and brain health, told Endpoints the company believed that genotyping patients is useful, though patients could still be treated without it.
 Wiesje van der Flier
Wiesje van der Flier“The monitoring and management of treatment is the same whether they’re homozygous or not,” he said.
But all of that adds to the burden for patients, even if it may help pinpoint the ones who could benefit the most with less risk.
“A lot of questions remain to be solved about this drug and its use,” Wiesje van der Flier, the scientific director of the Alzheimer Center Amsterdam at Amsterdam University Medical Centers in the Netherlands, said in an email.
“Which patients are most likely to benefit, and which patients are least likely to experience severe side effects?” van der Flier asked. “What are the optimal starting criteria — and perhaps even more importantly, when can we stop the treatment? And how does the slowing of progression translate to a patients’ daily functioning?”

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Scientists use organoid model to identify potential new pancreatic cancer treatment
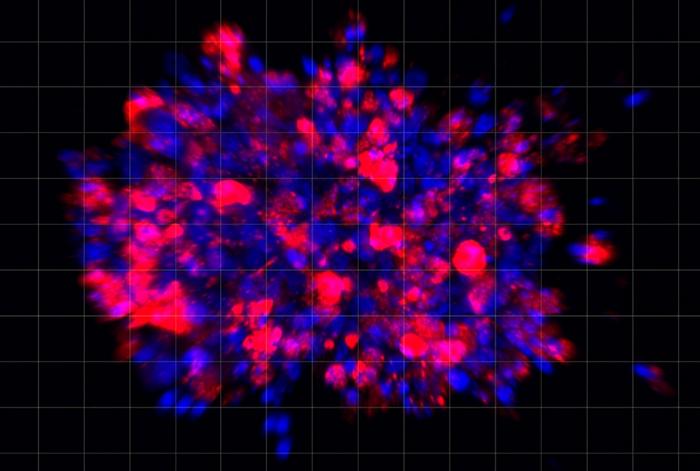
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…