Government
Digitally Transforming Clinical Trials
Digitization of clinical trials isn’t particularly new. Today, electronic data capture is only one of myriad technologies deployed in clinical trials…

Digitization of clinical trials isn’t particularly new. In the 1990s, the first iteration of electronic data capture (EDC) technology—then called remote data capture or RDC—was deployed to record clinical data onsite. But the early days of RDC weren’t exactly game-changing. While study data may have moved from paper to an electronic format, these systems were usually offline, capturing data only at each trial site. Like their paper report predecessors, data had to be collected and brought back to a central location for downloading.
Today, EDC is only one of myriad technologies deployed in clinical trials as drug sponsors and contract research organization look to develop vital insights and streamline clinical trials. Patient recruitment, qualifying patients, patient consent, drug efficacy and safety monitoring, as well as predictive modeling via machine learning and AI all play a role in modern drug studies. Leveraging mobile devices such as smartphones allows clinical trial managers to enhance patient engagement, while mobile health technologies that can capture real-time patient data or provide telehealth consultations has driven the growth in decentralized clinical trials (DCTs).

“Over the last 25 years, we started to see different approaches, incremental approaches to leverage technology in different ways to create new value propositions whether it be efficiency, whether it be cost savings, whether it be accelerating trials, or whether it be finding patients,” says Rohit Nambisan, CEO of Lokavant, a data driven clinical trial intelligence platform company. Today, Nambisan says his company and others are looking to leverage technology in novel ways to improve clinical trials but to also “reduce patient burden and site burden in the process as well.”
Patient recruitment and enrollment
Recruiting the right patients and enough of the right patients continues to hamper the management of clinical trials. A legacy hurdle to recruiting patients is a lack of comprehensive information available to treating physicians about current trial availability. In short, a doctor can’t refer a patient if they don’t know whether a trail appropriate for a patient even exists. Geographic constraints also affect patient recruitment. Clinical trial sites are typically clustered near large urban centers and traditional trials requiring regular site visits. According to a 2021 report by McKinsey & Company, 70% of eligible participants live more than two hours away from a clinical trial site, which places a significant burden on patients. In many instances, eligible patients simply don’t participate.
The result of this and other barriers is stark: only 5% of people eligible for any given trial participate and around 80% of clinical trials fail to meet their initial enrollment targets and timelines—delays that can cost pharma sponsors as much as $8 million per day in lost revenue.1 DCTs have the potential to address some of the root causes of low trial participation, but also to help improve equity in clinical research by removing geographic and trust barriers.
Patient recruitment is now moving online as drug sponsors leverage the power of social media and messaging to reach out to potential trial participants, while availability of claims data from payers and data contained in patients’ electronic health records (EHRs) allow for more focused recruitment efforts.
“One area of benefit [from leveraging digital technologies] is in patient finding,” Nambisan notes. “Being able to connect multiple data sources and leverage learning models can identify a needle in the haystack to drive recruitment, which drives efficiency and the cost of the trial.”

associate professor
Harvard’s T.H. Chan School of Public Health
Joseph Kvedar, MD, associate professor at Harvard’s T.H. Chan School of Public Health adds that digital methods of outreach also help lessen the burden on patients and trial sponsors alike. “There are efficiencies in recruiting people over various electronic platforms, whether it be Facebook, or email, or other methods,” he says. “Finding subjects is very expensive, then enrolling them and keeping them enrolled is also costly. You can make it easier for them to sign up this way, because they don’t want to come to a facility.”
Once patients have been recruited, gaining their consent for the research is the next, vital, step and electronic consent (eConsent) tools are fast becoming a method of choice not only for DCTs but other trials as well. “Traditionally, if you think you’re joining a trial, you’d be given a 50-page consent form that looked a lot like a legal contract,” says Andrew McKinnon, general manager of consent at Medable, a decentralized clinical trial platform provider. “I did an interview with some of our Patient Advisory Council and I asked those that had been in a trial to give a word that described their perception of the consent process. The one word that most of them came back with was: intimidating.”
Today’s eConsent applications allow patients to provide consent via their tablets, laptops, or cell phones and do it when it is convenient to them and not feel pressured by the time constraints of getting through a long written form while at the trial site. When accessing an eConsent, patients are provided with a range of media formats that describe the trial and their responsibilities. Videos, audio, interactive questions, and graphics not only provide the necessary information but are an early tool to foster patient engagement.

general manager of consent
Medable
“It’s a much less scary experience. People understand what they are signing up for and the result, from the perspective of those running the trial, is the patients are retained in the studies longer,” McKinnon notes. “It’s no longer a surprise for them when they have to come into the hospital every four weeks, which they may not have understood if they were just looking at some God-awful table embedded in a consent form.”
Ardy Arianpour, CEO and co-founder of patient healthcare data company Seqster, adds: “The big benefit of eConsent is it empowers patients to make informed decisions. Using interactive components improves efficiency of the clinical trial through insights into the patient experience. Because we not only allow patients to collect, own, and share their data, they’re also able to view their data—and that helps improve data quality.”
Leveraging mHealth Technology
Conducting DCTs essentially creates a need to leverage digital technologies. If the trials have a patient cohort that is more dispersed, fewer visits to physical trial sites are enhanced by telehealth visits. Currently, the most useful and accessible remote data from patients is provided from devices such as wearable fitness trackers, smart health watches, wearable glucose monitors, and blood pressure monitors, among others. These devices can provide a stream of real-time, real-world data to clinical trial teams that they haven’t had access to in the past. All these data can be used to help support whether a drug candidate is working and can also help sniff out adverse events.
“I think one way to look at the present is what are the limitations of the current generation of wearables, which are limited to vital signs and activity monitoring,” says Kvedar. “But my watch can do a pretty good job of saying I walked 1,000 steps, or when I’m in the gym at home matching my heart rate to my exertion. So, some of the clinical use cases for those might be in Parkinson’s disease or for people who are depressed where you can measure the success of your new antidepressant by measuring activity.”

Kvedar mentions the burgeoning area of weight loss medications whose effects can be remotely and digitally captured via blood pressure devices and blood sugar monitoring as another area or research that is benefitting from today’s available remote data capture technologies.
Looking into the future, he sees the potential for more than simply wearables as a means to feed useful data into clinical trials. “Another area I’m quite interested in is home testing,” Kvedar notes. “What can we do with a prick of your finger and drop of blood? Theranos notwithstanding, there are companies doing that in an honest way.” In the future, he envisions streams of data will flow from more than wearables and mobile devices and could even include weather data. “All of a sudden, you are getting this rich flow of data that can create a unique scenario around each one of us.”
With so much data already flowing into clinical trials today—and potentially more in future—are drug sponsors effectively using these data? “Now, you have continuous streams from data monitoring,” says Nambisan. “You re going to have to overlay that in some manner to understand the correlations. I think the existing data warehouses and systems are not well set up to handle that.”

CEO and co-founder, Seqster
Arianpour has a different view. “Pharma sponsors have expertise in analysis, but what they don’t have access to is the data itself,” he notes. “Now that we are providing access to all the data, they can leverage their expertise. What has been hard for pharma is it has taken years and billions of dollars for them to collect the wrong data. Now, they can cut through all that red tape.”
Regulatory concerns
With the volume of data generated passively by study participants, there need to be assurances that their data will be protected. At Medable, that means their consenting practices often need to be customized down to the site level to take into account local privacy and security regulations. Likewise, platforms for telemedicine are built to ensure security of the information and to be HIPAA compliant.
While platform companies providing remote patient data capture technologies need a technology backbone that protects patient privacy, the regulatory environment varies from country to country, with some regulations, such as the EU’s GDPR being more rigorous than others. “How you submit trials for approval and how you communicate that with the IRB, the ethics committee (EC) and what is acceptable, varies a lot between countries,” McKinnon notes. “For things like consent, in some countries it is eSign, in others it is print to sign. It is challenging particularly when you are looking at big, global studies.”
Regulatory bodies, however, are stepping up to meet the challenges presented by the growth in DCTs, including the FDA releasing a new guidance document in May and a toolkit developed over the course of 18 months by industry stakeholders in the U.S. intended to help sponsors manage the quality, privacy, and security of data in these trials. When digital health technologies are employed to collect health data remotely, as opposed to it occurring at a traditional clinical trial site, the toolkit notes that it is essentially adding an intermediary between the patient and the clinical investigator.
“Participant privacy is one of the key facets of an IRB/EC review in any clinical trial. In a trial using decentralized approaches, there are unique ethical considerations associated with a specific technology (e.g., telehealth, apps, and sensors) and with the providers who interact with participants in their homes or other locations away from the trial site,” the toolkit developers note. “Accordingly, an IRB/EC may need to review additional contract terms, processes, and potential vulnerabilities of participants’ private information, as well as participants’ knowledge of who will have access, how their private information may be used, and what choices they can make about these things.”
Kvedar adds that what he has observed, at least in the U.S. with the FDA, has been positive actions that don’t compromise privacy and security, even if some digital and mobile health device developers grumble about the limiting effects it may have on innovation.
“Maybe, in their minds, it is a drag on their progress,” Kvedar says regarding some device and software developers. “But we are talking about health. We’re talking about people’s lives, and we certainly don’t want to be entering things into the marketplace that could potentially be harmful. So, I’m balanced. I think (the FDA) is doing a good job.”
Chris Anderson, a Maine native, has been a B2B editor for more than 25 years. He was the founding editor of Security Systems News and Drug Discovery News, and led the print launch and expanded coverage as editor in chief of Clinical OMICs, now named Inside Precision Medicine.
The post Digitally Transforming Clinical Trials appeared first on Inside Precision Medicine.
contract research
pharma
healthcare
medicine
health
hospital
device
devices
digital health
ai
mobile health
mhealth
ehrs
telehealth
telemedicine
machine learning
apps
software
weight loss
public health
mobile
fitness
fda
research
clinical trials
clinical research

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
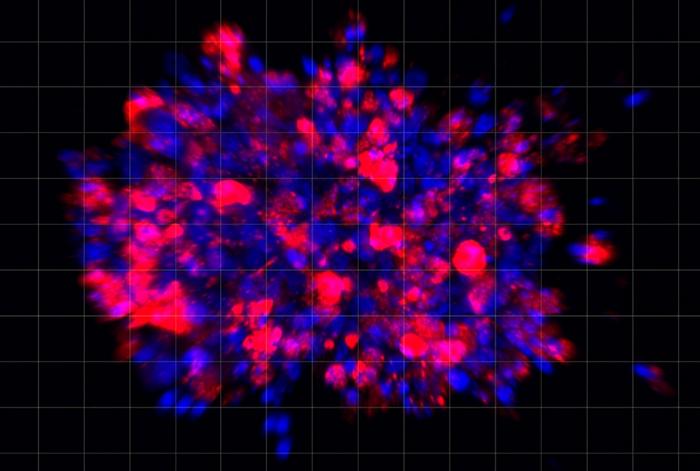
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…