Government
Making AAVs the Go-To for Making Gene Therapies Go
As gene therapy evolves to target additional indications—including more common indications—the choice of delivery platform is bound to become more…

By MaryAnn Labant
As gene therapy evolves to target additional indications—including more common indications—the choice of delivery platform is bound to become more interesting. At present, the most common delivery platform is the adeno-associated virus (AAV) vector. But there are, of course, other delivery platforms, and they can be expected to excel in certain contexts. Moreover, delivery platforms of all kinds are being refined. So, the primacy of AAVs is hardly assured.
We can be sure that AAVs have attractive qualities. After all, why else would five AAV-enabled gene therapies have received FDA approval? These therapies are as follows: Elevidys, from Serepta Therapeutics, for Duchenne muscular dystrophy; Hemgenix, from CSL Behring, for hemophilia B; Luxturna, from Spark Therapeutics, for retinal dystrophy; Roctavian, from BioMarin Pharmaceutical, for severe hemophilia A; and Zolgensma, from Novartis, for spinal muscular atrophy.

AAV advantages include injectability (for in vivo applications); high transduction efficiency; targetability (different serotypes for transducing different cell types); and relatively low genotoxicity and immunogenicity (compared with other viral vectors). However, AAVs have disadvantages, too.
One disadvantage is that AAV, as a naturally occurring virus, can still be expected to provoke immune responses in some patients. According to Soumi Gupta, PhD, senior director, head of clinical immunology, BioMarin, 30–60% of the population has measurable antibodies to different AAV serotypes from a wild-type infection.
Due to their impact on efficacy and safety, preexisting anti-AAV antibodies can restrict patient access to AAV-enabled gene therapies. In many clinical trials for such therapies, an excess of such antibodies is an accepted exclusion criterion. New immunomodulatory approaches and computational tools are in play to dampen or eliminate the immunogenicity of AAV vectors. Also, better targeting of AAVs could allow lower AAV doses, which would reduce toxicity from AAV immunity.
If AAV immunogenicity were reduced, other AAV disadvantages would become less, well, disadvantageous. For example, less immunogenic AAVs could be deployed in larger numbers to deliver large payloads piecemeal, overcoming the problem of limited cargo capacity. Also, less immunogenic AAVs could be safely deployed in multiple, sequential doses, helping resolve a problem related to nonreplication of AAV payloads, namely, transgene dilution.
It must be said, however, that even if immunogenicity could be contained, AAVs would pose manufacturing challenges such as productivity, cost, and scalability. In fact, these challenges could become more pressing if more treatments were to involve multiple doses, or if AAVs were to become more customized and less amenable to standardization.
Coping with AAV-specific antibodies
Currently, no assays exist to predict the development of an immune response to AAV-enabled gene therapy. Humoral or cellular adaptive immune responses target the capsid and/or the transgene-expressed protein product. In AAV-enabled gene therapies, the immune response is primarily directed toward the AAV capsid; however, both vector- and patient-specific factors impact how an immune system reacts.
Vector-specific factors include the capsid serotype, the clinical dose, the nature of the promoter, the size of the transgene, the manufacturing process (and process-related impurities), and the vector payload. Patient-specific factors include underlying disease mutations and disease-driven changes in the target tissue, as well as preexisting immunity to the vector and prior exposure to recombinant proteins. Other patient-specific factors include decisions over immunomodulation and route of vector administration.
“While every patient will develop antibodies, and many will develop a cellular response against the capsid, the development of an antibody response and/or a cellular response to the transgene-expressed protein is dependent on several factors,” Gupta says. “The most important is whether there is any endogenous expression of the target transgene in the patient population, which reduces the risk of an adaptive immune response.”
Two key types of assays are used for measuring preexisting antibodies against the AAV capsid. One assay is the cell-based transduction inhibition assay. It detects in vitro neutralizing capacity of antibodies and non-antibody neutralizing factors in plasma or serum. The other assay is the cell-free biochemical binding assay. It detects total anti-capsid binding antibodies in plasma or serum, regardless of neutralizing activity.
Preexisting AAV-specific neutralizing antibodies (NAbs) may reduce the efficacy of the dose administered and can directly inhibit transduction of the AAV gene therapy into the target cell by blocking binding of the vector to the AAV receptor. Both NAbs and non-NAbs can potentially impact biodistribution of the vector away from target cells by redirecting the vector to secondary lymphoid organs for clearance. In addition, anti-AAV NAbs challenge the administration of an efficacious second dose of therapy mediated by the same AAV serotype.
“Some researchers have suggested that including empty capsids in the product can serve as a decoy for the antibodies,” Gupta notes. “Others have considered increasing treatment dose to overwhelm the antibody concentration.”
Ordinarily, the presence of empty capsids in clinical-grade AAVs is avoided because empty capsids can increase antigen load and T-cell activation. However, antigen presentation can be limited if empty capsids are modified so that they cannot enter target cells but are still able to absorb antibodies.
BioMarin is investigating additional hypotheses and approaches, including strategies that temporarily remove or degrade preexisting antibodies prior to therapy administration through in vivo enzymatic degradation or apheresis using size-exclusion or affinity chromatography. Gupta emphasizes that intervention strategies for removing, clearing, or inhibiting antibodies prior to dose administration could increase the population of patients eligible for first and subsequent doses.
Improving capsids, promoters, and cell lines
Although the immune response to the administration of AAV vectors remains a challenge, scientists are improving their ability to manage immunogenicity. As a result, more AAV-enabled gene therapies are advancing in clinical programs and achieving regulatory approval.
“We believe we have developed the technology required to potentially achieve positive patient outcomes,” asserts Canwen Jiang, MD, PhD, chief development officer and chief medical officer, Asklepios BioPharmaceutical (AskBio). “Work pioneered by our co-founder and CSO Jude Samulski, PhD, has contributed to the development of approved AAV gene therapies for spinal muscular atrophy (type 1), retinal dystrophy, and other diseases.” Jiang notes that these therapies are being delivered to patients by other companies. He adds that under Samulski’s scientific leadership, AskBio continues to advance multiple AAV product programs to clinical stage.
According to Jiang, for some AAV clinical development programs, the practice is to exclude patients with preexisting immunities. Another is to deliver AAV vectors via specific routes of administration to select organs that are less likely to be affected by immunogenicity. AAV therapies can also include treatments with immune inhibitors and modulators.
“We have developed AAV vector delivery platforms for central nervous system and cardiovascular indications,” Jiang reports. “[These platforms can] minimize potential negative impacts of immunogenicity on efficacy and safety.”
Samulski has been pioneering foundational scientific research to further understand the molecular mechanisms underlying AAV vector immunogenicity. For example, he has led projects to discover novel vectors, as well as projects to optimize expression cassettes. In such projects, the aim is to reduce immunogenicity and improve efficacy.
Yet other projects focus on manufacturing. In these projects, the goal is to enhance scalability. “That is one reason why we invested in manufacturing,” Jiang says. “Samulski and our chief technology officer, Josh Grieger, PhD, developed our Pro10-based suspension manufacturing platform. It is used by our CDMO subsidiary Viralgen Vector Core and its clients.”
According to Jiang, AskBio is “at the forefront of gene therapy thanks to groundbreaking research, our advanced manufacturing capabilities, synthetic promoter and enzymatic DNA technology, a library of chimeric capsids, and more than 800 patents and patent applications in areas such as AAV production and chimeric and self-complementary capsids.” The company has delivered positive data from Phase I studies in Parkinson’s disease and congestive heart failure, and it has clinical trials in limb-girdle muscular dystrophy type 2I/R9, Huntington’s disease, Pompe disease, and multiple system atrophy.
Combining computational design and in vitro testing
In AAV-enabled gene therapies, an antibody landscape influenced by preexisting immunity is as important as an adaptive immune response. “We are also becoming increasingly aware that existing natural immunity to AAVs may be a source of previously unexplained serious autoimmunity or immune-mediated illnesses in certain populations,” says Steve Goldfless, PhD, head of technology and strategy, G:Labs, Generate Biomedicines. “Using our protein design capability based on our artificial intelligence/machine learning (AI/ML) platform, we have the ability to eliminate certain epitopes of interest that are recognized by NAbs while retaining the structure and function of the viral vector.”

lab in Andover, MA.) [Lara Woolfson, Studio Nouveau]
Generate Biomedicines also uses an in vitro cell culture system. Once put into the AI/ML platform, the generated data recapitulate the ability of the human body to mount an immune response. The platform can also predict sequences to tune down and make an immune response less efficient against an engineered construct. For some molecules, this process is informed by cryogenic electron microscopy (cryo-EM) structures.
“We start with the computational prediction, then we use in vitro testing to hone and refine it,” explains Alexandra Snyder, MD, executive vice president, R&D, Generate Biomedicines. “This is a gradual de-risking process, but ultimately you need the human data to know how to deal with immunogenicity in the clinical context.”
Preexisting antibodies prevent the therapy from working sustainably. “In some cases, you can dose over it so that the antidrug antibodies do not prevent the therapy from accomplishing efficacy,” Snyder continues. “However, this can lead to some of the potential toxicities associated with these therapies. Eliminating or greatly reducing human recognition can open the window and lead to lower toxicity risk.”
Certain key steps in recognizing a foreign antigen and the immune response are known; others are not. For example, existing technology is broadly used to engineer around immunogenic class I peptides. “This is one specific step in the process, but one can capture high-quality data and then use sophisticated computational modeling to generate predictions,” Goldfless suggests. “For other steps, complete understanding and models are still being developed. To work around this, we generate high-quality, large-scale laboratory data and learn on it.”
AI/ML platforms can process and integrate very large amounts of data to gain the ability to recognize patterns that a human cannot. Usually, drug development is a stepwise process addressing variables sequentially. “Our approach allows simultaneous changes,” Snyder asserts. “To develop therapies that work across a diversity of patients, the capability to de-risk immunogenicity is essential.”
Introducing in silico de-risking systems
In 2014, the FDA issued its first guidance to address the immunogenicity risks posed by therapeutic proteins. The principal author of the guidance, Amy Rosenberg, MD, was the director of the Division of Therapeutic Proteins, Center for Drug Evaluation and Research. She recalls that “protein therapy was at the forefront, cell therapy was in play, but gene therapy was just emerging.” Today, Rosenberg is the senior director of immunology and protein therapeutics at EpiVax.
Rosenberg observes that the use of protein therapeutics can be complicated by immune responses. To support this point, she describes what was learned after patients with infantile-onset Pompe disease (IOPD)—a rare, fatal, lysosomal storage disease in which the lysosomal enzyme a-glucosidase is deficient or entirely absent—began receiving an enzyme replacement therapy (ERT) called Lumizyme. Responses to the Lumizyme, researchers determined, partly depended on cross-reactive immunologic material (CRIM) status.
CRIM-positive patients had some partly functional endogenous a-glucosidase protein. They were tolerant to and benefitted from the ERT long term. CRIM-negative patients lacked endogenous protein. They developed robust immune responses to the ERT, regressed, and eventually died.
CRIM status, researchers recognized, had to be considered when Lumizyme was administered to IOPD patients. For example, Duke University’s Priya S. Kishnani, MD, led work to implement an immune tolerance protocol to improve outcomes in IOPD patients. When an AAV-mediated gene therapy with a liver-specific promoter was later developed at Duke University, patients had humoral tolerance to the transgene but not to the AAV capsid even though they were treated with steroids that prevented cytolytic responses to the capsid.
“Young patients will require retreatment,” Rosenberg points out. “If patients have a significant anti-AAV antibody titer, the antibodies must be eliminated, or they prevent transduction of the cell population of interest.” To eliminate the antibodies, protocols have been implemented that address the development of humoral responses to AAV viral capsids.
“Immunogenicity is a broad problem,” Rosenberg continues. “Currently, there are several approaches to management depending on the disease and the nature and extent of the treatment, but no single approach covers all possibilities.” Moreover, various preclinical methods exist for assessing and mitigating immunogenicity, allowing drug developers to proactively de-risk their pipelines.

One method is in silico analysis. It is based on the amino acid sequence of a biologic and can be used for assessment of any format of biologic, including many of the new modalities such as gene/cell therapies, multispecific antibodies, fusion proteins, novel peptides, and others.
EpiVax has pioneered this space with its flagship ISPRI (Interactive Screening and Protein Re-engineering Interface) toolkit, an industry standard for measuring immunogenicity. ISPRI tools can be used to investigate known T-cell epitope sequences and develop a more accurate picture of risk. This includes the evaluation of regional immunogenicity and the identifiction of what EpiVax calls Tregitopes—epitopes that can be tolerated or actively tolerogenic due to cross-conservation. ISPRI tools can also be leveraged to de-immunize and tolerize sequences to mitigate potential immunogenicity issues.
The post Making AAVs the Go-To for Making Gene Therapies Go appeared first on GEN – Genetic Engineering and Biotechnology News.
manufacturing
therapeutics
antibodies
cell therapy
gene therapy
biopharmaceutical
chromatography
medical
artificial intelligence
ai
machine learning
pharmaceutical
fda
research
clinical trials

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
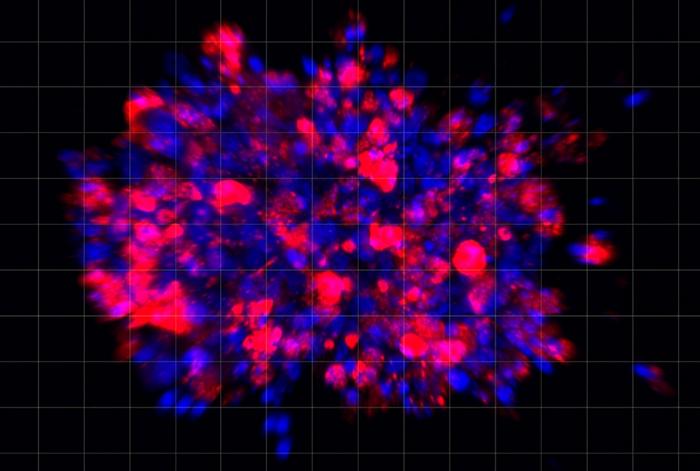
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…