Government
Mechanism Underpinning “Chemo-Brain” Identified, Points to Existing Drug as Potential Therapy
Patients receiving cancer chemotherapy often experience long-lasting cognitive impairments, dubbed “chemo brain.” Studies by scientists at Saint Louis…

Patients receiving cancer chemotherapy often experience what can be debilitating side effects, including cognitive impairments in processing speed, memory, executive function and attention. Dubbed “chemo brain,” these lingering symptoms can dramatically impact patients’ quality of life long after they have completed their cancer treatments. Currently, there are no FDA-approved drugs for treating such side effects.
Scientists at Saint Louis University, led by pain researcher Daniela Salvemini, PhD, the William Beaumont professor of pharmacology and physiology, and department Chair, have now uncovered some of the molecular events that may underlie these chemotherapy-related deficits. The team described study results demonstrating what they suggest is the first evidence that chemotherapy alters a key cellular pathway, sphingolipid metabolism, in critical areas of the brain linked to cognitive function. The research, including experiments in mice, links chemotherapy-related cognitive impairments (CRCI) with increased levels of the signalling molecule sphingosine-1-phosphate (S1P), and suggest that an existing FDA-approved S1P receptor 1 (S1PR1) antagonist drug that is used to treat multiple sclerosis also appear to reduce chemotherapy-related cognitive impairment. “Our findings are fascinating since two functional S1PR1 antagonists are already FDA-approved for treating multiple sclerosis,” Salvemini said. “Repurposing these drugs to prevent CRCI would be a ground-breaking shift towards enhancing patient quality of life in cancer treatment.”
The team reported on its findings in Journal of Clinical Investigation, in a paper titled “Sphingosine-1-phosphate receptor 1 activation in the central nervous system drives cisplatin-induced cognitive impairment,” in which they concluded, “Collectively, our results identify the molecular mechanisms engaged by the S1P/S1PR1 axis in CRCI and establish S1PR1 antagonism as an approach to target CRCI with therapeutics that have fast-track clinical application.”
The National Cancer Institute (NCI) expects cancer survivorship to reach 21.7 million by 2029, the researchers noted. And as greater numbers of patients survive cancer there is also an increasing need to address the severe, long-lasting neurotoxic side effects of chemotherapy.
Chemotherapeutics, including taxanes such as paclitaxel and platinum-based agents such as cisplatin, are widely used as part of standard treatment for numerous cancers, including head and neck, testicular, colon, breast, ovarian and non-small cell lung cancers. CRCI is a major neurotoxic side effect of chemotherapy, and can profoundly affect quality of life. As the authors noted, “Cancer-related cognitive impairment (CRCI) is a major neurotoxicity affecting more than 50% of cancer survivors … Reported cognitive deficits affect up to 75% of patients treated with chemotherapy for cancers outside the nervous system.”
However, the authors continued, “Our current understanding of the mechanisms underlying CRCI and their impact on cognition is limited, due to the multifactorial origins of CRCI.” Salvemini, who is also director of the Henry and Amelia Nasrallah Center for Neuroscience at SLU and a fellow of the Saint Louis Academy of Science, added, “A better understanding of these mechanisms is essential for developing new therapies and improving survivors’ quality of life.”

Salvemini had previously pioneered research on a treatment for neuropathic pain that could provide the first alternative to ineffective steroids and addictive opioids. Work from Salvemini’s lab established that altered S1PR1 signaling in the central nervous system in response to chemotherapy contributes to chemotherapy-induced neuropathic pain. This work fueled two ongoing NCI clinical trials to test the potential use of Gilenya (FTY720), a drug approved to treat multiple sclerosis, to prevent neuropathic pain in patients with breast cancer treated with paclitaxel.
“We previously showed that two chemotherapeutic agents, paclitaxel and bortezomib, cause dysregulation of de novo sphingolipid metabolism in the spinal cord that led to development of chemotherapy-induced neuropathic pain, another major cancer-treatment neurotoxicity,” the investigators noted. “These earlier findings prompted us to examine the effects of cisplatin on sphingolipid metabolites in the CNS, the team noted in their newly reported study.
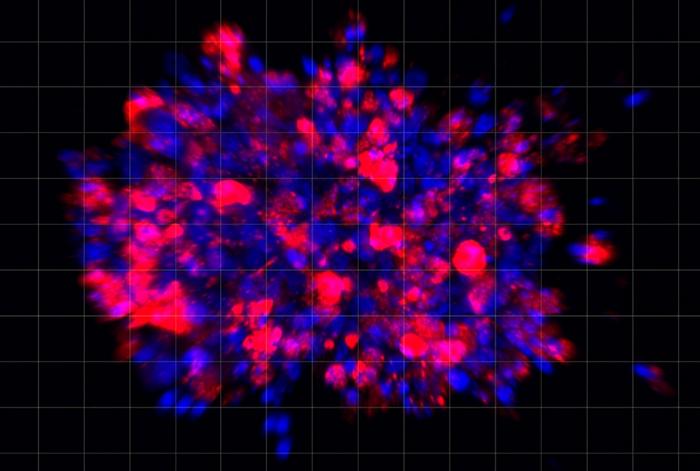
Through this newly reported research the team found that in the central nervous system, cisplatin increases levels of S1P, which contributes to the development of CRCI through activation of S1PR1 on astrocytes and S1PR1-driven mitochondrial dysfunction and neuroinflammatory processes. The studies also revealed that mechanistically, cisplatin-induced S1P formation is mediated by the toll-like receptor 4.
“In mice that developed CRCI, we found a significant increase in TLR4 expression in the PFC [prefrontal cortex] and hippocampus,” the investigators commented. And importantly, cisplatin therapy did not induce CRCI in mice treated using a TLR4 inhibitor, or in knockout mice lacking TLR4 (Tlr4-/- animals). In the Tlr4-/- animals cisplatin did not increase SIP levels in the PFC and hippocampus. “We believe this is the first study implicating TLR4 activation as a causal mechanism for CRCI,” they noted. “Our studies provide evidence that TLR4 activation in the brain is the linchpin in cisplatin-induced S1P formation, S1P-mediated S1PR1 activation, and cognitive deficits.”
The findings bridge some gaps in scientists’ understanding about the molecular mechanisms underlying CRCI, and identify a novel target for therapeutic intervention with functional S1PR1 antagonists. Importantly, S1PR1 antagonists do not interfere with the efficacy of chemotherapy, as the team, and others, have shown in previous work, and can also block tumor cell growth, inflammation and metastasis. “Noteworthily, several preclinical studies suggest that FTY720 does not negatively interfere with the therapeutic activity of chemotherapeutics, including cisplatin, and also possesses anticancer activity by blocking tumor growth and metastasis,” the investigators stated.
They further concluded in their paper, “Building on a compelling preclinical platform, future clinical trials are needed to assess the anticancer effects of S1PR1 antagonists given alone or in combination with chemotherapy. Repurposing these drugs to prevent CRCI would be a ground-breaking shift toward enhancing patient quality of life in cancer treatment.”
Salvemi added, “Our work is very translational. We try to understand the mechanisms at the molecular level, identify the targets, work with our chemists to make new drugs to target that specific pathway, test it, and then take the necessary steps to move along this compound until it is ready to be studied in a clinical trial.”
The post Mechanism Underpinning “Chemo-Brain” Identified, Points to Existing Drug as Potential Therapy appeared first on GEN – Genetic Engineering and Biotechnology News.
therapeutics
application
therapy
fda
research
clinical trials

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…