Government
The Fast Pace of Cancer Research is Leaving Community Clinicians Behind
Corey Zankowski, CEO of Primum We are witnessing an accelerated pace of amazing breakthroughs and advancements in cancer care today, with new treatments…


We are witnessing an accelerated pace of amazing breakthroughs and advancements in cancer care today, with new treatments emerging almost weekly and unprecedented opportunities to help improve patient outcomes every day. However, if a doctor is not working in an academic setting, reading every new paper, and recruiting patients for new studies, how can they be expected to keep up with the latest treatments and approaches to specific cancers? When a community oncologist sees a patient with an unfamiliar cancer diagnosis, they need a way to get timely, trusted advice on the best treatment plan. We have a tremendous opportunity to use modern technology to share medical information, and I’d like to examine some promising approaches to exchange knowledge between Academic Medical Centers (AMC) and Community Oncology Practices (COP).
Breakthroughs in molecularly targeted therapies and immunotherapy have revolutionized the cancer treatment landscape for patients. More than 50 novel anti-cancer therapies were approved in 2020, a five-fold increase over the past decade. That’s almost one new therapy a week. While the pace of progress is impressive, the need for care is also increasing. The CDC estimates that the number of cancer cases will increase by 49%, from 1.5 million annually in 2015 to 2.3 million in 2050.
There are approximately 13,365 licensed oncologists in the US today, and only 10.5% of those physicians practice in rural areas, according to the American Society of Clinical Oncology’s 2022 workforce snapshot. At the same time, about 80% of cancer care occurs in community health centers.
The community oncologists who provide the majority of cancer care may treat a wide variety of malignancies every day, and may often see 30 patients with 30 different diagnoses per day – a vast range of diseases and potential treatments. Many therapeutics target a particular gene mutation or specific protein and are paired with diagnostic tests that probe tumor cells or blood for these biomarkers. Knowing which new treatment is best for a specific patient can require overwhelming work by COP doctors to stay up to date on a broad range of cancer types.
Patients living in rural areas can also find it challenging to see a specialist. The National Rural Health Association found that in urban areas, there are about 263 general specialists per 100,000 people – but only 30 in rural areas. This gap severely restricts the ability for patients to meet with subspecialists or find out about new trials.
In the 2000’s, HIPAA mandated standardized EHRs, which enabled more efficient medical care (eventually). The COVID-19 pandemic pushed many in the medical community to utilize telehealth technologies for safer patient interactions. While there is no question that oncology has become very high-tech, when it comes to digital communication, it is as if the revolution in mobile devices, social networking and information technology has passed medicine by.
Doctors may be able to scan forums, pour over guidelines and read academic papers, but the ability to find the right solution for a particular patient often requires advice from their local network of COP colleagues. Yet, most patients cannot receive the latest cancer treatments without having access to oncology subspecialists based at an AMC. If we really want to work towards improving the health care system, we need better ways to share information that improves outcomes in community settings.
Today’s options – curbside consults, tumor boards, external referrals
Community oncologists need answers fast when they face a tricky treatment decision. It can be a matter of life or death. Cancer is uniquely complex, with many types and sub-types, and every patient has distinct circumstances. Cancer’s complexity makes it challenging for a community oncologist to decide between multiple treatment paths, unless they have expertise in that specific cancer subtype.
Finding the right oncology subspecialists can be nearly impossible for community oncologists working within their limited personal networks. When faced with a quandary in deciding on a treatment plan without local support, many doctors either refer patients to subspecialists or submit their cases to a formal tumor board for guidance. Sending a patient to subspecialists may involve hundreds of miles in travel and weeks away from home for many patients, and should be used only after thoughtful consideration. At the same time, organizing and scheduling a tumor board to review one case is cumbersome, requiring the coordination of the schedules for multiple practitioners. Moreover, a tumor board may not get scheduled according to the patient’s ideal timeline. When clinicians need quick advice about the best treatment option for their patients, many take advantage of the so-called “curbside consult” and ask their immediate peers for feedback.
Tumor boards and typical curbside consults pull from a limited pool of colleagues. A “curbside” gets its name from the serendipitous hallway or sidewalk meeting of two colleagues, and not from the targeted insight of a physician with deep knowledge of the patient’s issue. Worse, tumor boards and hallway meetings are both “synchronous” approaches to knowledge sharing – requiring all parties to meet in real-time to address the problem – making scheduling more difficult. Patient care should not depend on the convenient relationships of their physician. Rather, it should benefit from the latest knowledge about the patient’s diagnosis and treatment.
Doctors can confer within their own medical group, yet there is currently no efficient means for treating oncologists to access the knowledge they need about the most innovative treatments across the field of medicine. An “asynchronous” communication method borrowed from email and other online communication might allow doctors to address questions on their own schedule. Existing technology can be used to virtualize the curbside consult and the traditional tumor board.
Connecting COPs and AMCs can improve outcomes
Several projects have looked at connecting experts over large distances via remote consultations. Recent innovations are producing effective ways to share knowledge in a HIPAA-compliant context. The best approach I’ve seen comes from several pilot programs connecting community HCPs with outside experts and researchers. In addition to providing new options, COPs may be able to enroll patients in specific new trials so their patients can access the latest available medical treatments.
These programs have all helped to mitigate setting-based discrepancies by helping AMCs and COPs collaborate via e-consultations and video conferencing. This approach is especially beneficial for doctors working in rural areas like the U.S. Southwest or Rocky Mountain region. Imagine how challenging it can be for patients in rural towns to access specialized care.
Project ECHO was created to ensure the right knowledge exists at the right place at the right time for patients, initially focused on hepatitis C in New Mexico. A recent scoping review of Project ECHO looked at 15 studies that connected remote doctors to centralized specialists and found that this approach eliminated almost half of ER visits. The authors noted, “For patients in rural communities, the limited presence of specialists can be a significant barrier to comprehensive, appropriate, accessible and timely care.” The review found that approximately half of the presented cases resulted in immediate changes in the care of the patients whose cases were reviewed.
Can this same approach achieve similar results within oncology? I believe it can.
COVID-19 introduced new challenges for healthcare providers. Social distancing, masking, and staff shortages dramatically impacted our ability to deliver high-quality care. Furthermore, routine screening and preventive medicine visits were delayed, resulting in more advanced disease, and negatively impacting cancer outcomes. Practice standards changed during the pandemic with the expansion of remote medicine, shorter treatment regimens and delayed elective treatments. The cancer community has adapted to COVID-19 by adopting new technologies and accelerating the utilization of digital health solutions. However, these changes raise even more questions from community oncologists.
AccessHope by the City of Hope studied how remote experts can provide better treatment recommendations for COPs. One key innovation for the program was the use of an asynchronous review of patient records by subspecialists, who then wrote a report listing potential treatment options for the local oncologist to consider. The program identified evidence-based protocols that changed the patient’s treatment in 28% of the 101 patients studied, and suggested improvements to the treatment plan in 92% of patients.
We believe that the asynchronous peer communication introduced by AccessHope improves upon traditional meeting formats that are so cumbersome for busy clinicians. However, a one-time expert review and opinion where local doctors can receive recommendations, but not necessarily ask follow-up questions disincline COP physicians from interactive dialog with AMCs. An ideal solution would permit asynchronous iterations between the community oncologists and the subspecialist.
Earlier this year Cigna announced a program with the National Cancer Institute, connecting community oncologists with national subspecialty experts within the insurer’s network. An initial pilot found that among the reviewed cases, 40% of patients with complex cancers benefited from updated treatment guidance.
When we look at the many challenges facing oncology care, from an increasing population of patients to a steady flow of novel treatments, there’s a clear need to connect COPs and AMCs across practices so community doctors can benefit from the latest knowledge coming from academic experts.
We see glimmers of hope in some of these ongoing and pilot projects, mainly driven by the rapid growth in options and the expansion of telehealth and remote treatment delivery methods. We can text a friend on the other side of the world today, but finding the right oncology subspecialists is still a challenge – we need to change this.
Cancer is one of the most fragmented, specialized, and complex medical fields today. Community oncologists deliver excellent cancer care in the local setting, but as generalists, it is impossible to keep pace with the rapid changes across all subspecialties. A modern, informed, and efficient process can improve outcomes for cancer patients and care providers.
If we bridge experiential insights from subspecialized oncologists with on-the-ground insights from community oncologists, we can improve outcomes for cancer patients across the country.
We have an opportunity to help eliminate the disparity in cancer care for populations living outside of major medical centers. This will directly impact the care of thousands of patients, create new ways to accelerate the spread of knowledge across the medical community and advance oncology care for everyone. The scale of the problem is only going to grow.
About Corey Zankowski
Corey Zankowski, Ph.D., is CEO & Co-Founder of Primum, a platform that connects community oncologists with oncology sub-specialists to help with complex treatment
decisions and accelerate the adoption of new and innovative therapies. Corey possesses over 20 years of experience in the oncology medical device industry. His vision and ability to execute in technology innovation have shaped the field of radiation oncology.
therapeutics
immunotherapy
biomarkers
medical
healthcare
diagnostic
medicine
health
delivery
device
devices
digital health
ehrs
telehealth
mobile
therapy
research
cdc

Here Are the Champions! Our Top Performing Stories in 2023
It has been quite a year – not just for the psychedelic industry, but also for humanity as a whole. Volatile might not be the most elegant word for it,…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
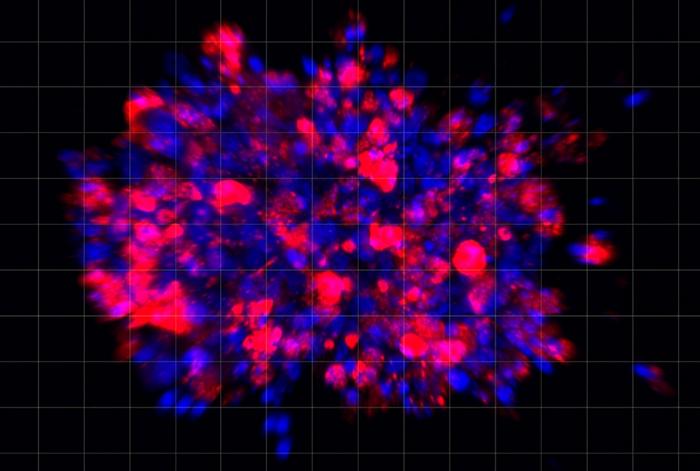
Scientists use organoid model to identify potential new pancreatic cancer treatment
A drug screening system that models cancers using lab-grown tissues called organoids has helped uncover a promising target for future pancreatic cancer…