Digital Health
Immunotherapy Failure Linked to Intratumoral Heterogeneity
New research has shed light on why immune checkpoint blockade immunotherapy does not always work in some cancers with a high tumor mutational burden. The…
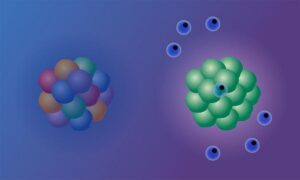
The results of a study led by researchers at EMBL’s European Bioinformatics Institute (EMBL-EBI), Cold Spring Harbor Laboratory (CSHL), and Massachusetts Institute of Technology (MIT), have shed light on why immune checkpoint blockade (ICB) immunotherapy does not always work in some cancers with a high tumor mutational burden (TMB). The researchers used mouse models and cell lines, and analyzed clinical trial data from human cancer patients, to identify the molecular mechanisms causing resistance to ICB in tumors with DNA mismatch repair deficiency (MMRd). While these types of tumors are generally among those that are the most sensitive to ICB therapy, results from the new study showed that intratumoral heterogeneity of mutations (ITH)—a wide variety of mutations spread across the tumor—dampens the immune response, leading to diminished effectiveness of the ICB treatment even among MMRd tumors. The investigators say their results provide important context for understanding immune evasion in cancers with a high TMB, and could have major implications for therapies that are designed to increase TMB.
“This is an important body of work that provides new insights into the factors that control immune responses against cancer and why some tumors fail to respond to immune-stimulating therapies,” said Tyler Jacks, PhD, professor at the Koch Institute at MIT. Jacks is co-senior and co-corresponding author of the team’s published paper in Nature Genetics, which is titled, “Mismatch repair deficiency is not sufficient to elicit tumor immunogenicity.”
Immunotherapy has been hugely successful for some forms of cancer, with notable success in tumors with a high number of mutations, including tumors with clonal neoantigens. Clonal neoantigens occur when identical mutations are present across all cells of a tumor. As the authors stated, “Immunotherapy has revolutionized the treatment landscape of many cancers, particularly those with a high tumor mutational burden (TMB).” Studies have found TMB to be one of the strongest predictors of ICB response, and one anti-PD-1 treatment has been approved by FDA for all tumors, based on high TMB alone, the investigators pointed out. MMRd is associated with some of the highest TMBs, and has shown “remarkable response rates” to ICB.
Even so, only about half of the MMRd tumors respond to ICB, and among responders, many will relapse, the researchers pointed out. Understanding what happens at the cellular level could help clinicians predict which patients are more likely to respond and guide treatment decisions. “Our goal was to unravel the mystery of why certain tumors, which should respond to immunotherapy, do not,” said Peter Westcott, PhD, assistant professor at Cold Spring Harbor Laboratory, and former postdoctoral researcher at MIT.
For their reported study, the researchers used preclinical mouse models, cell lines, as well as clinical trial data from colon and gastric cancer patients to analyze tumor responses to ICB.
Through studies in mouse models, the team demonstrated that inactivation of MMR is not enough to improve patient responsiveness to ICB. They found that mouse models of MMRd lung and colon cancers, “surprisingly,” didn’t display increased T-cell infiltration or response to ICB. This the authors commented, was the result of “substantial intratumor heterogeneity of mutations.” Westcott noted, “There’s no question these tumors are MMRd, yet they’re not responding. That is a profoundly interesting negative result.”

When the team then evaluated the clinical data, they also observed that colon and stomach tumors with a diluted mutational signal caused by intratumoral heterogeneity displayed reduced sensitivity to ICB treatment. This finding suggests that identifying the level of signal strength in individual tumors could help predict a patient’s response to ICB in the clinic. “By studying the mechanisms behind this resistance, we can pave the way for the development of more effective and personalized treatment strategies,” Westcott added.
ICB functions by obstructing an immune checkpoint—a signal exploited by cancer cells to stop the immune system from detecting the tumor through the high number of mutations found within these cancer cells. Such mutations can serve as cues that enable the immune system to identify and combat the tumor. In the context of ICB, weaker mutation signals lead to a diminished response to treatment because the immune system has a harder time finding and recognizing the cancer cells.
“One way to picture this is to imagine a crowd, where each person is holding a yellow flashlight,” explained Isidro Cortes-Ciriano, PhD, research group leader at EMBL-EBI. “If everyone turns on their flashlight, the beam of yellow light can be seen from far away. Similarly, the more cells with the same mutations in a tumor, the stronger the signal and the more likely to trigger an immune response. However, if each person in the crowd has a different colored flashlight, the light emanating from the crowd is less clear, and the signal becomes jumbled. Similarly, if cancer cells have different mutations, the signal is harder to make out and the immune system is not triggered, so ICB doesn’t work.”
The findings of this study highlight the pivotal role played in this process by intratumoral heterogeneity. “This is an important body of work that provides new insights into the factors that control immune responses against cancer and why some tumors fail to respond to immune-stimulating therapies,” said Tyler Jacks, PhD, professor at the Koch Institute at MIT.
Findings from the study provide a means to identify which patients are more likely to benefit from ICB treatment, highlighting the need for personalized treatment approaches. “Our understanding of cancer is improving all the time, and this translates into better patient outcomes,” added Cortes-Ciriano. “Survival rates following a cancer diagnosis have significantly improved in the past twenty years, thanks to advanced research and clinical studies. We know that each patient’s cancer is different and will require a tailored approach. Personalized medicine must take into account new research that is helping us understand why cancer treatments work for some patients but not all.”
The post Immunotherapy Failure Linked to Intratumoral Heterogeneity appeared first on GEN – Genetic Engineering and Biotechnology News.

Keep it Short
By KIM BELLARD OK, I admit it: I’m on Facebook. I still use Twitter – whoops, I mean X. I have an Instagram account but don’t think I’ve ever posted….
Asian Fund for Cancer Research announces Degron Therapeutics as the 2023 BRACE Award Venture Competition Winner
The Asian Fund for Cancer Research (AFCR) is pleased to announce that Degron Therapeutics was selected as the winner of the 2023 BRACE Award Venture Competition….
Seattle startup Olamedi building platform to automate health clinic communications
A new Seattle startup led by co-founders with experience in health tech is aiming to automate communication processes for healthcare clinics with its software…













