Wellness
Diet and Exercise? Some Clinicians Don’t Have Time to Cover Them: The Healthcare Satisfaction Survey
Many people with diabetes do not get the holistic, all-encompassing care that the condition requires.
Diabetes touches nearly every aspect of life. It’s been said that type 1 diabetes impacts well over a hundred decisions per day, and type 2 diabetes can be just as all-consuming, especially for those that use insulin. Many members of our community divide their lives in two — before and after their diagnosis — because diabetes simply changes everything.
How can doctors, endocrinologists, and nurse practitioners hope to address the totality of this condition? Can they help their patients refine not just their medication use but also their diets, their exercise, their sleep habits, their mental health? Frankly, the truth is that they probably can’t, and a growing national shortage of healthcare providers is not helping.
We know that many people with diabetes believe that their healthcare providers can help with only some of the diabetes puzzle. We wanted to measure how Americans with diabetes feel about the care they’re getting right now.
The Healthcare Satisfaction Survey
On Nov. 4, in celebration of Diabetes Awareness Month, we announced the completion of a new survey that aimed to assess how satisfied regular Americans with diabetes are with the medical care and attention they receive. We collaborated on the effort with our friends at Thrivable, a market research platform that engages panels of people with chronic health conditions.
Diabetes is tough, and we know that not everyone gets the support they need. As one of our panelists put it: “They make it seem like it’s an easy thing to do to manage diabetes, with little consideration of stress and financial levels.” We wanted to measure how people with diabetes feel about the care they get from their healthcare providers.
This is the third of three articles that will explore the many amazing things that we learned from the Healthcare Satisfaction Survey. These three deep dives are organized around the most jaw-dropping results:
- 47.1 percent of people with diabetes rarely or never discuss mental health at healthcare appointments.
- Black and Latino people with diabetes are about half as likely to feel supported or empowered at healthcare appointments as white patients.
- 22.7 percent of people with diabetes rarely or never discuss diet or exercise with their healthcare providers, and about 50 percent rarely or never discuss their lab results.
The Context: Doctors and Nurses Are Stretched Thin
The United States does not have enough doctors and nurses. There are wide reports of shortages among family doctors, registered nurses, and endocrinologists.
According to the latest government accounting, nearly 100 million Americans live in health professional shortage areas (HPSAs). This problem can be especially acute in rural areas: Some members of the Diabetes Daily community live hours from the closest endocrinologist. But even those in denser areas can find it nearly impossible to get an appointment.
Almost everyone agrees that physicians do not spend enough time with their patients. A recent study found that primary care physicians would need to work about 27 hours per day in order both to see an average number of patients and to meet national care guidelines.
Unfortunately, the problem appears to be getting worse, especially in diabetes care. Given the growth of diabetes rates, a huge public health problem even before the COVID-19 pandemic caused diabetes cases to mysteriously skyrocket, the gap between supply and demand is only likely to grow.
The negative results are predictable for both patient and doctor alike: “suboptimal access … reduced time spent face to face, and poor communication. … The net outcome is reduced patient satisfaction, and depersonalization and ultimately burnout for clinicians.”
This context is important when reviewing the results of our Healthcare Satisfaction Survey, which will show that some people with diabetes are probably not getting the care they deserve. Undoubtedly, many doctors and nurses wish that they could spend more time with each patient but are prevented from doing so by a healthcare system over which they have no control.
One of our panelists put it this way:
“When needing to discuss multiple things with my endocrinologist/nurse practitioner, I often feel rushed due to the allotted time of the appointment. I feel this is a corporate or insurance-driven directive …”
The Thrivable Panel
Our 532 survey panelists were selected by Thrivable to create a nationally representative sample. The participants hailed from all parts of the United States, were of all different ages, and were both racially/ethnically and socioeconomically diverse. Our participants held many different types of insurance coverage, including Medicare, Medicaid, private insurance, marketplace insurance, and employee insurance. Some had no insurance at all.
About 60 percent of the panel had type 2 diabetes, and most of the rest had type 1.
The Results: Diet, Weight, and Exercise
There’s no doubt about it: Diet is absolutely fundamental to diabetes care. “Comprehensive” dietary change is part of the first line of treatment for people with type 2 diabetes, and people with type 1 diabetes quickly learn that their condition requires careful consideration of practically every mouthful that they take for the rest of their lives. For many of us, life with diabetes is largely defined by what it means for our eating habits.

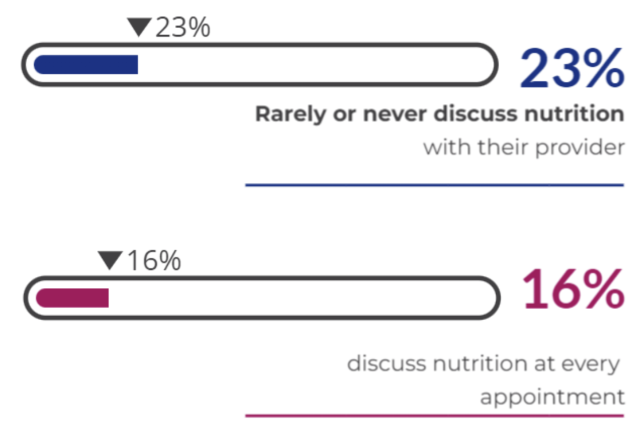
Imagine our surprise when 22.7 percent of our panelists reported they rarely (17.0 percent) or never (5.7 percent) discuss nutrition, diet, or ways of eating at their healthcare appointments. Here’s how that number breaks down:
- Respondents with type 1 diabetes were more likely to report that they “rarely” or “never” discuss nutrition with their healthcare providers than respondents with type 2 (26.6 percent and 18.8 percent, respectively).
- General practitioners (27.5 percent of visits) and nurse practitioners (24.1 percent) were reportedly more likely to rarely or never discuss nutrition, compared with endocrinologists (20.1 percent), certified diabetes care and education specialists (16.1 percent), and diabetes coaches (9.1 percent).
Exercise is, like diet, part and parcel of the comprehensive lifestyle modifications that are recommended as the first line of treatment for people with type 2 diabetes. If there’s a single guideline that every diabetes expert can agree on, it’s that exercise is an essential element of optimum type 2 diabetes health. The recommendation applies to almost everyone, even the elderly and those living with conditions like painful neuropathy that make exercise difficult. Even very light exercise like walking or gardening has huge benefits.
Exercise is a big deal for people with type 1 diabetes, too, not only because it helps metabolic health so much, but also because exercise can be so tricky to manage properly.
And yet, the numbers were broadly similar for the topic of exercise, with a substantial minority of panel members telling us that they rarely or never discuss the topic at healthcare appointments.
- 21 percent of respondents reported rarely or never discussing exercise with their providers.
- General practitioners (45.0 percent) and nurse practitioners (36.2 percent) were the least likely to discuss the topic “often” or “always.”
To be clear, a strong majority of panelists did discuss these topics with their caretakers at least as often as “sometimes.” Nevertheless, given the centrality of diet and exercise to diabetes management, we were surprised by the substantial minority of patients who did not frequently discuss them.
The pattern of responses also lends validity to the theory we began to develop in our examination of the survey data on racial, ethnic, and socioeconomic disparities in care: that as diabetes patients become wealthier, they are increasingly able to access a team of specialists to optimize their care.
Our survey suggested that endocrinologists are more likely to discuss diet and nutrition than generalists like family doctors and nurse practitioners. We can only speculate as to the reason — it may simply be that endocrinologists have more time. Primary care providers, after all, must care for all of a patient’s healthcare needs.
Not every person with diabetes has access to an endocrinologist. One of our panelists stated that they had to self-advocate to get endo appointments:
“My diabetes is complicated by other comorbidities. I have learned to insist on management by an endocrinologist and their team rather than a GP [general practitioner].”
Meanwhile, diabetes coaches and CDCESs are even more likely than endos to discuss these important lifestyle-based therapies. These providers may have less advanced training than doctors and nurses, but can specialize in the nitty-gritty of life with diabetes. In our panel, unfortunately, almost nobody earning less than $50,000 saw one of these professionals. The same goes for registered dieticians, who were all but unavailable to our panelists with the lowest reported incomes. The result is a topsy-turvy situation in which patients with less money likely receive less instruction on diet and exercise, the least expensive diabetes therapies out there.
Weight
Weight is an inextricable element of health for most people with type 2 diabetes. Surprisingly, our survey showed that people with type 1 diabetes were more likely to report that their healthcare provider always measured their weight at appointments than those with type 2 (85.6 and 56.8 percent, respectively).
This may seem backward at first glance; type 2 diabetes is the condition highly associated with obesity, not type 1. It’s tough to explain the gap. But this surprising difference may actually represent a wise approach to diabetes and weight. There are movements, both among patients and clinicians alike, to put a halt to routine weighing at the doctor’s office. A precise weight measurement is not typically medically necessary, and most of us don’t need to look at a scale to know if we have some weight to lose. Diabetes is already associated with the incidence of eating disorders; stepping on the scale can just add unnecessary anxiety to a doctor’s appointment.
Our theory is supported by the fact that patients with type 1, though they were more likely to step on a scale, said they were much less likely to actually discuss their weight with their healthcare providers. Among those with type 1, only 28.5 percent reported “often” or “always” having conversations about weight management, compared with nearly 50 percent of those with type 2. That number may rise in the future — though sustainable weight loss sometimes seems impossible, experts are increasingly admitting that weight loss is the key to diabetes treatment.
Lab Results and Blood Pressure
Our panel revealed some other surprising disparities between type 1 and type 2 diabetes:
- 87 percent of respondents with type 1 diabetes stated that they “often” or “always” discuss lab results with their doctors, compared with only 67 percent of those with type 2.
- 87 percent of those with type 1 diabetes stated that their provider “always” checks their blood pressure, compared with only 55 percent of those with type 2.
We’re not sure how to explain this discrepancy and whether it’s meaningful. Both type 1 and type 2 are evaluated substantially through the use of laboratory results — most significantly, an A1C measurement — and both predispose patients to cardiovascular illness, which makes hypertension especially dangerous.
Takeaways
The healthcare providers who treat diabetes are badly overworked, and they don’t have enough time to advise their patients on the type of holistic, all-encompassing treatment that life with diabetes truly demands. That may be especially true of generalists like primary care physicians and nurse practitioners, who have even less time to devote to diabetes care.
Our survey indicates that one result of this unfortunate dynamic is that too many people with diabetes receive little or no advice on the important topics of nutrition and exercise.
Several of our panelists even confessed that they go to their medical appointments as rarely as possible, because they don’t feel like these visits offer much benefit:
“I have excellent results mainly based on my own set of goals, research, pump/CGM knowledge, etc. At this point, my Medicare mandated quarterly meetings with my CDCES are just to make sure I can get my prescriptions renewed/boxes checked. While we have a good relationship, I don’t receive the level of care that I would like to make MY relatively minor diabetes challenges less obtrusive to MY daily life. I’m tired of being held up as the star of the practice.”
“I actually hate going to the doctor and avoid it. I go only to have my prescriptions renewed … I feel like she just wants to get me in and out and move on to our next patient. … The only reason why I know anything is because I look it up myself.”
The Diabetes Daily Healthcare Satisfaction Survey suggests that endocrinologists and other specialists (including dieticians, diabetes educators, and diabetes coaches) are able to offer more comprehensive care that is better targeted to the needs of people with diabetes. Unfortunately, these experts are unavailable or beyond the means of many patients.

Lion’s Mane Mushroom: History, Benefits, and Adaptogen Properties
Explore the intriguing world of Lion’s Mane Mushroom in our comprehensive guide. Dive into its unique properties, historical significance, and myriad health…
AI can already diagnose depression better than a doctor and tell you which treatment is best
Artificial intelligence (AI) shows great promise in revolutionizing the diagnosis and treatment of depression, offering more accurate diagnoses and predicting…
Reasons You should Get this: Neptune Wellness Solutions Inc (NASDAQ:NEPT), WeTrade Group Inc. (NASDAQ:WETG)
NEPT has seen its SMA50 which is now -9.28%. In looking the SMA 200 we see that the stock has seen a -92.25%. WETG has seen its SMA50 which is …
The…













